16.1 Fertilisation
Learning Objectives
By the end of this section, you will be able to:
- Describe the obstacles that sperm must overcome to reach an oocyte to enable fertilisation
- Explain capacitation and its importance in fertilisation
- Summarise the events that occur as a sperm fertilises an oocyte in order to form a zygote
- Explain the artificial reproductive technologies (ART) that are used for assisted reproduction in humans
Fertilisation occurs when a sperm and an oocyte (egg) combine and their nuclei fuse. Because each of these reproductive cells is a haploid cell containing half of the genetic material needed to form a human being, their combination forms a diploid cell. This new single cell, called a zygote, contains all the genetic material needed to form a human – half from the mother and half from the father.
Transit of Sperm
Fertilisation is a numbers game. During ejaculation, hundreds of millions of sperm (spermatozoa) are released into the vagina. Almost immediately, millions of these sperm are overcome by the acidity of the vagina (approximately pH 3.8) and millions more may be blocked from entering the uterus by thick cervical mucus. Of those that do enter, thousands are destroyed by phagocytic uterine leukocytes. Thus, the race into the uterine tubes, which is the most typical site for sperm to encounter the oocyte, is reduced to a few thousand contenders. Their journey—thought to be facilitated by uterine contractions—usually takes from 30 minutes to two hours. If the sperm do not encounter an oocyte immediately, they can survive in the uterine tubes for another 3–5 days. Thus, fertilisation can still occur if intercourse takes place a few days before ovulation. In comparison, an oocyte can survive independently for only approximately 24 hours following ovulation. Intercourse more than a day after ovulation will therefore usually not result in fertilisation.
During the journey, fluids in the female reproductive tract prepare the sperm for fertilisation through a process called capacitation or priming. The fluids improve the motility of the spermatozoa. They also deplete cholesterol molecules embedded in the membrane of the head of the sperm, thinning the membrane in such a way that will help facilitate the release of the lysosomal (digestive) enzymes needed for the sperm to penetrate the oocyte’s exterior once contact is made. Sperm must undergo the process of capacitation in order to have the “capacity” to fertilise an oocyte. If they reach the oocyte before capacitation is complete, they will be unable to penetrate the oocyte’s thick outer layer of cells.
Contact Between Sperm and Oocyte
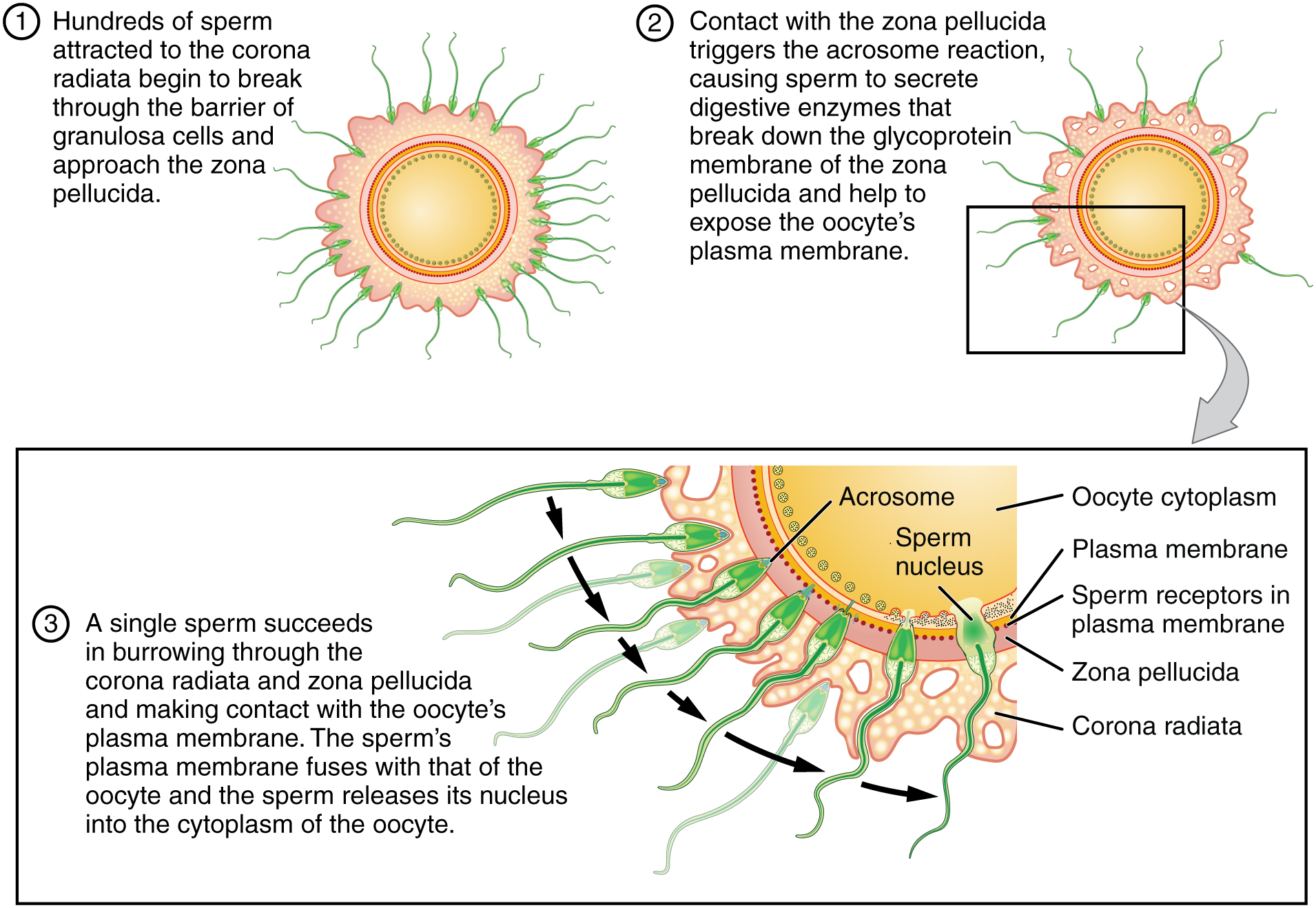
Upon ovulation, the oocyte released by the ovary is swept into—and along—the uterine tube. Fertilisation must occur in the distal uterine tube because an unfertilised oocyte cannot survive the 72-hour journey to the uterus. As you will recall from your study of the oogenesis, this oocyte (specifically a secondary oocyte) is surrounded by two protective layers. The corona radiata is an outer layer of follicular (granulosa) cells that form around a developing oocyte in the ovary and remain with it upon ovulation. The underlying zona pellucida (pellucid = “transparent”) is a transparent, but thick, glycoprotein membrane that surrounds the cell’s plasma membrane.
As it is swept along the distal uterine tube, the oocyte encounters the surviving capacitated sperm, which stream toward it in response to chemical attractants released by the cells of the corona radiata. To reach the oocyte itself, the sperm must penetrate the two protective layers. The sperm first burrow through the cells of the corona radiata. Then, upon contact with the zona pellucida, the sperm bind to receptors in the zona pellucida. This initiates a process called the acrosomal reaction in which the enzyme-filled “cap” of the sperm, called the acrosome, releases its stored digestive enzymes. These enzymes clear a path through the zona pellucida that allows sperm to reach the oocyte. Finally, molecules on the sperm head of a single sperm contact the sperm-binding receptors on the oocyte’s plasma membrane (Figure 16.1.1). The plasma membrane of that sperm then fuses with the oocyte’s plasma membrane, and the head and mid-piece (not the tail) of the “winning” sperm enter the cytoplasm (interior) of the oocyte.
How do sperm penetrate the corona radiata? Some sperm undergo a spontaneous acrosomal reaction, which is an acrosomal reaction not triggered by contact with the zona pellucida. The digestive enzymes released by this reaction digest the extracellular matrix of the corona radiata. As you can see, the first sperm to reach the oocyte is never the one to fertilise it. Rather, hundreds of sperm cells must undergo the acrosomal reaction, each helping to degrade the corona radiata and zona pellucida until a path is created to allow one sperm to contact and fuse with the plasma membrane of the oocyte. If you consider the loss of millions of sperm between entry into the vagina and degradation of the zona pellucida, you can understand why a low sperm count can cause male infertility.
When the first sperm fuses with the oocyte, the oocyte deploys two mechanisms to prevent polyspermy, which is penetration by more than one sperm. This is critical because if more than one sperm were to fertilise the oocyte, the resulting zygote would be a triploid organism with three sets of chromosomes. This is incompatible with life.
The first mechanism is the fast block, which involves a near instantaneous change in sodium ion permeability upon binding of the first sperm, depolarising the oocyte plasma membrane and preventing the fusion of additional sperm cells. The fast block sets in almost immediately and lasts for about a minute, during which time an influx of calcium ions following sperm penetration triggers the second mechanism, the slow block. In this process, referred to as the cortical reaction, cortical granules sitting immediately below the oocyte plasma membrane fuse with the membrane and release zonal inhibiting proteins and mucopolysaccharides into the space between the plasma membrane and the zona pellucida. Zonal inhibiting proteins cause the release of any other attached sperm and destroy the oocyte’s sperm receptors, thus preventing any more sperm from binding. The mucopolysaccharides then coat the nascent zygote in an impenetrable barrier that, together with hardened zona pellucida, is called a fertilisation membrane.
The Zygote
Recall that at the point of fertilisation, the oocyte has not yet completed meiosis; all secondary oocytes remain arrested in metaphase of meiosis II until fertilisation. Only upon fertilisation does the oocyte complete meiosis. The unneeded complement of genetic material that results is stored in a second polar body that is eventually ejected. At this moment, the oocyte has become an ovum, the female haploid gamete. The two haploid nuclei derived from the sperm and oocyte and contained within the egg are referred to as pronuclei. They decondense, expand, and replicate their DNA in preparation for mitosis. The pronuclei then migrate toward each other, their nuclear envelopes disintegrate, and the male- and female-derived genetic material intermingles. This step completes the process of fertilisation and results in a single-celled diploid zygote with all the genetic instructions it needs to develop into a human.
Most of the time, a woman releases a single egg during an ovulation cycle. However, in approximately 1 percent of ovulation cycles, two eggs are released, and both are fertilised. Two zygotes form, implant, and develop, resulting in the birth of dizygotic (or fraternal) twins. Because dizygotic twins develop from two eggs fertilised by two sperm, they are no more identical than siblings born at different times.
Much less commonly, a zygote can divide into two separate offspring during early development. This results in the birth of monozygotic (or identical) twins. Although the zygote can split as early as the two-cell stage, splitting occurs most commonly during the early blastocyst stage, with roughly 70–100 cells present. These two scenarios are distinct from each other, in that the twin embryos that separated at the two-cell stage will have individual placentas, whereas twin embryos that form from separation at the blastocyst stage will share a placenta and a chorionic cavity.
Everyday Connections
In Vitro Fertilisation (IVF)
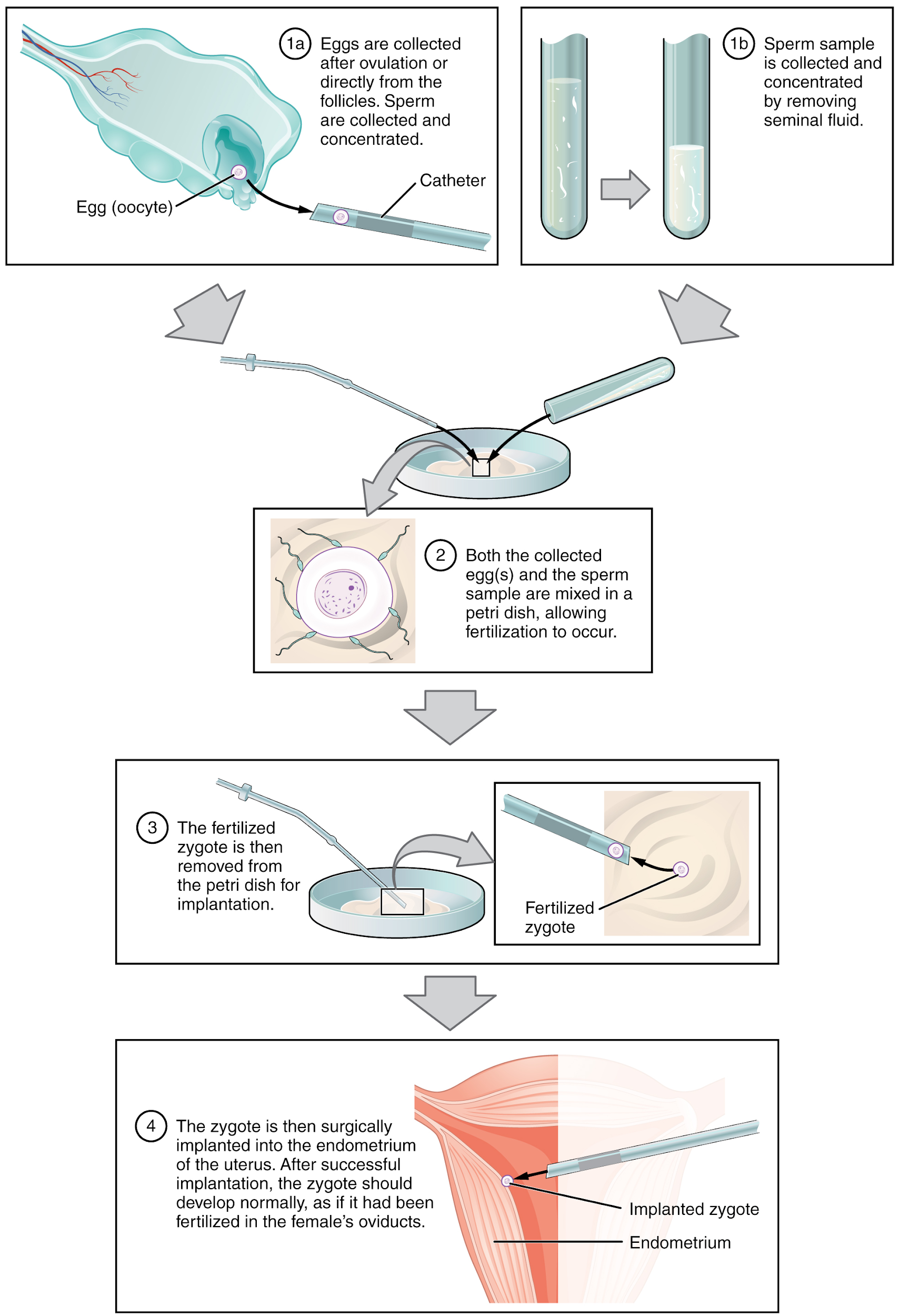
IVF, which stands for in vitro fertilisation, is an assisted reproductive technology. In vitro, which in Latin translates to “in glass,” refers to a procedure that takes place outside of the body. There are many different indications for IVF, for example, a woman may produce normal eggs, but the eggs cannot reach the uterus because the uterine tubes are blocked or otherwise compromised. A man may have a low sperm count, low sperm motility, sperm with an unusually high percentage of morphological abnormalities, or sperm that are incapable of penetrating the zona pellucida of an egg.
A typical IVF procedure begins with egg collection. A normal ovulation cycle produces only one oocyte, but the number can be boosted significantly (to 10–20 oocytes) by administering a short course of gonadotropins. The course begins with follicle-stimulating hormone (FSH) analogs, which support the development of multiple follicles, and ends with a luteinising hormone (LH) analog that triggers ovulation. Right before the ova would be released from the ovary, they are harvested using ultrasound-guided oocyte retrieval. In this procedure, ultrasound allows a physician to visualise mature follicles. The ova are aspirated (sucked out) using a syringe.
In parallel, sperm are obtained from the male partner or from a sperm bank. The sperm are prepared by washing to remove seminal fluid because seminal fluid contains a peptide, FPP (or, fertilisation promoting peptide), that—in high concentrations—prevents capacitation of the sperm. The sperm sample is also concentrated, to increase the sperm count per millilitre.
Next, the eggs and sperm are mixed in a petri dish. The ideal ratio is 75,000 sperm to one egg. If there are severe problems with the sperm—for example, the count is exceedingly low, or the sperm are completely nonmotile, or incapable of binding to or penetrating the zona pellucida—a sperm can be injected into an egg. This is called intracytoplasmic sperm injection (ICSI).
The embryos are then incubated until they either reach the eight-cell stage or the blastocyst stage. In most countries, for example Australia, UK, US and Canada, fertilised eggs are typically cultured to the blastocyst stage because this results in a higher pregnancy rate. Finally, the embryos are transferred to a woman’s uterus using a plastic catheter (tube). Figure 16.1.2 illustrates the steps involved in IVF.
The first successful IVF procedure was conducted in 1973. Seven years later, in 1980, the first IVF birth in Australia occurred. In 1983 the world saw the first birth from a frozen embryo prior to transfer. Despite the advances and milestones reached over the last 50 years, IVF technology is a continuously evolving technique.
The rate of success for IVF is correlated with a woman’s age. In Australia, the success rate for live births from fresh embryo transfers is approximately 40% in patients 30 years and younger, however drops to only approximately 9% in women over the age of 40. Similarly, the rate of live births from frozen embryo transfer is approximately 35% in women 30 years and younger and approximately 27% in women 40 years and older.
Career Connection
IVF Scientist/Embryologist
The IVF or Fertility Clinics industry in Australia and world-wide is growing as more couples decide to delay pregnancy. Medical facilities in this industry offer services such as assisted reproductive technologies (ART) including IVF, frozen embryo transfer, fertility treatments, intrauterine insemination and donor insemination as well as diagnostic and genetic testing. An IVF Scientist or Embryologist requires a minimum of a bachelor’s degree in biomedical science or biological science focussing on human biology.
Section Review
Hundreds of millions of sperm deposited in the vagina travel toward the oocyte, but only a few hundred reach it. The number of sperm that reach the oocyte is greatly reduced because of conditions within the female reproductive tract. Many sperm are overcome by the acidity of the vagina, others are blocked by mucus in the cervix, whereas others are attacked by phagocytic leukocytes in the uterus. Those sperm that do survive undergo a change in response to those conditions. They go through the process of capacitation, which improves their motility and alters the membrane surrounding the acrosome, the cap-like structure in the head of a sperm that contains the digestive enzymes needed for it to attach to and penetrate the oocyte.
The oocyte that is released by ovulation is protected by a thick outer layer of granulosa cells known as the corona radiata and by the zona pellucida, a thick glycoprotein membrane that lies just outside the oocyte’s plasma membrane. When capacitated sperm make contact with the oocyte, they release the digestive enzymes in the acrosome (the acrosomal reaction) and are thus able to attach to the oocyte and burrow through to the oocyte’s zona pellucida. One of the sperm will then break through to the oocyte’s plasma membrane and release its haploid nucleus into the oocyte. The oocyte’s membrane structure changes in response (cortical reaction), preventing any further penetration by another sperm and forming a fertilisation membrane. Fertilisation is complete upon unification of the haploid nuclei of the two gametes, producing a diploid zygote.
Review Questions
Critical Thinking Questions
Click the drop down below to review the terms learned from this chapter.
