1.10 Medication Safety
Now that the basic concepts of medication onset, peak, and duration have been discussed, it is important to understand the value of the therapeutic window and therapeutic index in medication administration.
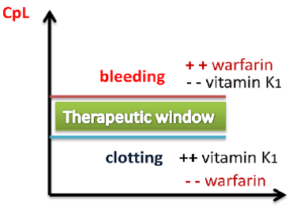
Therapeutic Window
For every drug, there exists a dose that is minimally effective (the Effective Concentration) and another dose that is toxic (the Toxic Concentration). Between these doses is the therapeutic window, where the safest and most effective treatment will occur (see Figure 1.7).[1] Think of this area as the dosing “sweet spot.”
For example, warfarin (Coumadin) is a medication used to prevent blood clotting and is monitored using a blood test called INR. Too high of a dose of warfarin would cause the INR to increase above the therapeutic window and put the patient at risk of bleeding. Conversely, too low of a dose of warfarin would cause the INR to be below the therapeutic window and put the patient at risk of clotting. It is vital that the nurse frequently monitors INR levels for a patient receiving warfarin to ensure the dosage appropriately reaches the therapeutic window and does not place the patient at risk for bleeding or clotting.
Peak and Trough Levels
Now let’s apply the idea of therapeutic window to the administration of medications requiring the monitoring of peak and trough levels, which is required in the administration of some IV antibiotics. It is important for the dosage of these medications to be titrated to achieve a desired therapeutic effect for the patient. Titration is often accomplished by closely monitoring the blood levels of the medication. A drug is said to be within the “therepeutic window” when the serum blood levels of an active drug remain consistently above the level of effective concentration (so that the medication is achieving its desired therapeutic effect) and consistently below the toxic level (so that no toxic effects are occurring). A peak drug level is drawn at the time when the medication is being administered and is known to be at the highest level in the bloodstream. A trough level is drawn when the drug is at its lowest in the bloodstream right before the next dose is given. Medications have a predicted reference range of normal values for peak and trough levels. These numbers assist the pharmacist and provider in gauging how the body is metabolizing, protein-binding, and excreting the drug, and assist in the adjustment of the prescribed drug doses to keep the medication within the therapeutic window. When administering IV medications that require peak or trough levels, it is vital for the nurse to time the administration of the medication according to the timing of these blood draws. [2]
Therapeutic Index
Therapeutic Index is a quantitative measurement of the relative safety of a drug. It is a comparison of the amount of drug that produces a therapeutic effect versus the amount of drug that produces a toxic effect.
- A large (or high) therapeutic index number means there is a large therapeutic window between the effective concentration and the toxic concentration of a medication, so the drug is relatively safe.
- A small (or low) therapeutic index number means there is a small therapeutic window between the effective concentration and the toxic concentration. A drug with a narrow therapeutic range (i.e., having little difference between toxic and therapeutic doses) often has the dosage titrated according to measurements of the actual blood levels achieved in the person taking it. For example, patients who start taking phenytoin to control seizures have the drug levels in their blood stream measured frequently.
Critical Thinking Activity 1.10a
Mr. Parker has been receiving gentamicin 80 mg IV three times daily to treat his infective endocarditis. He has his gentamicin level checked one hour after the end of his previous gentamicin infusion was completed. The result is 30 mcg/ml. Access the link below to determine the nurse’s course of action.
View information on Therapeutic Drug Levels
(Within the activity link, be sure to select “click to keep reading” in order to view drugs that are commonly checked, their target levels, and what abnormal results mean).
Based on the results in the above patient scenario, what action will the nurse take based on the result of the gentamicin level of 30 mcg/mL?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” sections at the end of the book.
- "Therapeutic Window" by Shefaa Alasfoor is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Principles of Pharmacology by LibreTexts licensed under CC BY-NC-SA 4.0. ↵
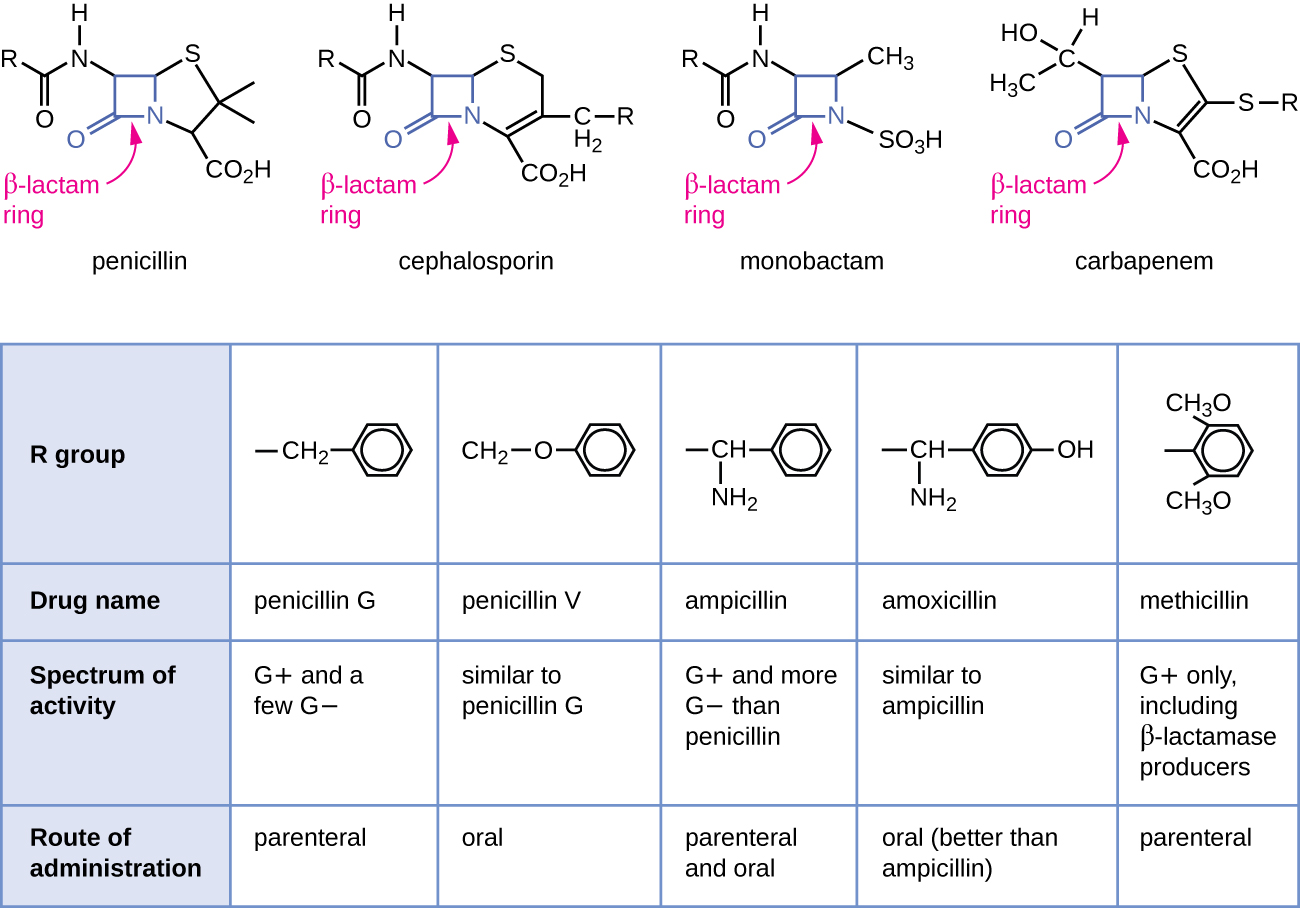
Cephalosporins are a slightly modified chemical "twin" to penicillins due to their beta lactam chemical structure. (See Figure 3.8 for a comparison of the beta-lactam ring structure, spectrum of activity, and route of administration across different classes of medications.) Because of these similarities, some patients who have allergies to penicillins may experience cross-sensitivity to cephalosporins.
Indications: Cephalosporins are used to treat skin and skin-structure infections, bone infections, genitourinary infections, otitis media, and community-acquired respiratory tract infections.
Mechanism of Action: Cephalosporins are typically bactericidal and are similar to penicillin in their action within the cell wall. Cephalosporins are sometimes grouped into "generations" by their antimicrobial properties. The 1st-generation drugs are effective mainly against gram-positive organisms. Higher generations generally have expanded spectra against aerobic gram-negative bacilli. The 5th-generation cephalosporins are active against methicillin-resistant Staphylococcus aureus (MRSA) or other complicated infections. [1]
Specific Administration Considerations: Patients who are allergic to pencillins may also be allergic to cephalosporins. Patients who consume cephalosporins while drinking alcoholic beverages may experience disulfiram-like reactions including severe headache, flushing, nausea, vomiting, etc.[2] Additionally, like penicillins, cephalosporins may interfere with coagulability and increase a patient's risk of bleeding. Cephalosporin dosing may require adjustment for patients experiencing renal impairment. Blood urea nitrogen (BUN) and creatinine should be monitored carefully to identify signs of nephrotoxicity.
Patient Teaching & Education: Patients who are prescribed cephalosporins should be specifically cautioned about a disulfiram reaction, which can occur when alcohol is ingested while taking the medication. Additionally, individuals should be instructed to monitor for rash and signs of superinfection (such as black, furry overgrowth on tongue; vaginal itching or discharge; loose or foul-smelling stool) and report to the prescribing provider.
It is also important to note that cephalosporin can enter breastmilk and may alter bowel flora of the infant. Thus, use during breastfeeding is often discouraged.[3]
Now let's take a closer look at the cephalosporin medication grid in Table 3.6.[4]
Table 3.6 Cephalosporin Medication Grid
Class/Subclass |
Prototype/Generics |
Administration Considerations |
Therapeutic Effects |
Side/Adverse Effects |
|---|---|---|---|---|
| Cephalosporins | 1st generation:
2nd generation: 3rd generation: 4th generation: 5th generation: |
Check for allergies, including if allergic to penicillin
Dosage adjustment if renal impairment Use with caution with seizure disorder PO: Administer without regard to food; if GI distress, give with food IV: Reconstitute drug with sterile water or normal saline; shake well until dissolved. Inject into large vein or free-flowing IV solution over 3-5 minutes Drug interaction: anticoagulants |
Monitor for systemic signs of infection:
-WBCs - Fever Monitor actual site of infection Monitor culture results, if obtained |
Common side effects:
-Nausea -Vomiting -Epigastric distress -Diarrhea Monitor for: -Rash -C-diff Nephrotoxicity if pre-existing renal disease Elevated INR and bleeding risk Development of hemolytic anemia |
Critical Thinking Activity 3.6a
Using the above grid information, consider the following clinical scenario question:
Mrs. Jenkins is an 89-year-old patient admitted to the medical surgical floor for treatment of a skin infection. The admitting provider prescribes Cefazolin 1 gram every 8 hours IV.
Mrs. Jenkins' admission laboratory tests include renal laboratory studies reflecting:
Creatinine: 1.3 mg/dL (Normal range: 1.2 mg/dL[5]
Blood urea nitrogen (BUN): 25 mg/dL (Normal: 8-20 mg/dL)
Glomerular Filtration Rate: 55 ml/min (Normal: 90-120 ml/min)[6]
On Day 3 Mrs. Jenkins has renal laboratory studies performed again. The results are:
Creatinine: 1.6 mg/dL
Blood urea nitrogen (BUN): 57 mg/dL
Glomerular Filtration Rate: 20 ml/min
Are Day 3 findings expected or not? What course of action should the nurse take?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
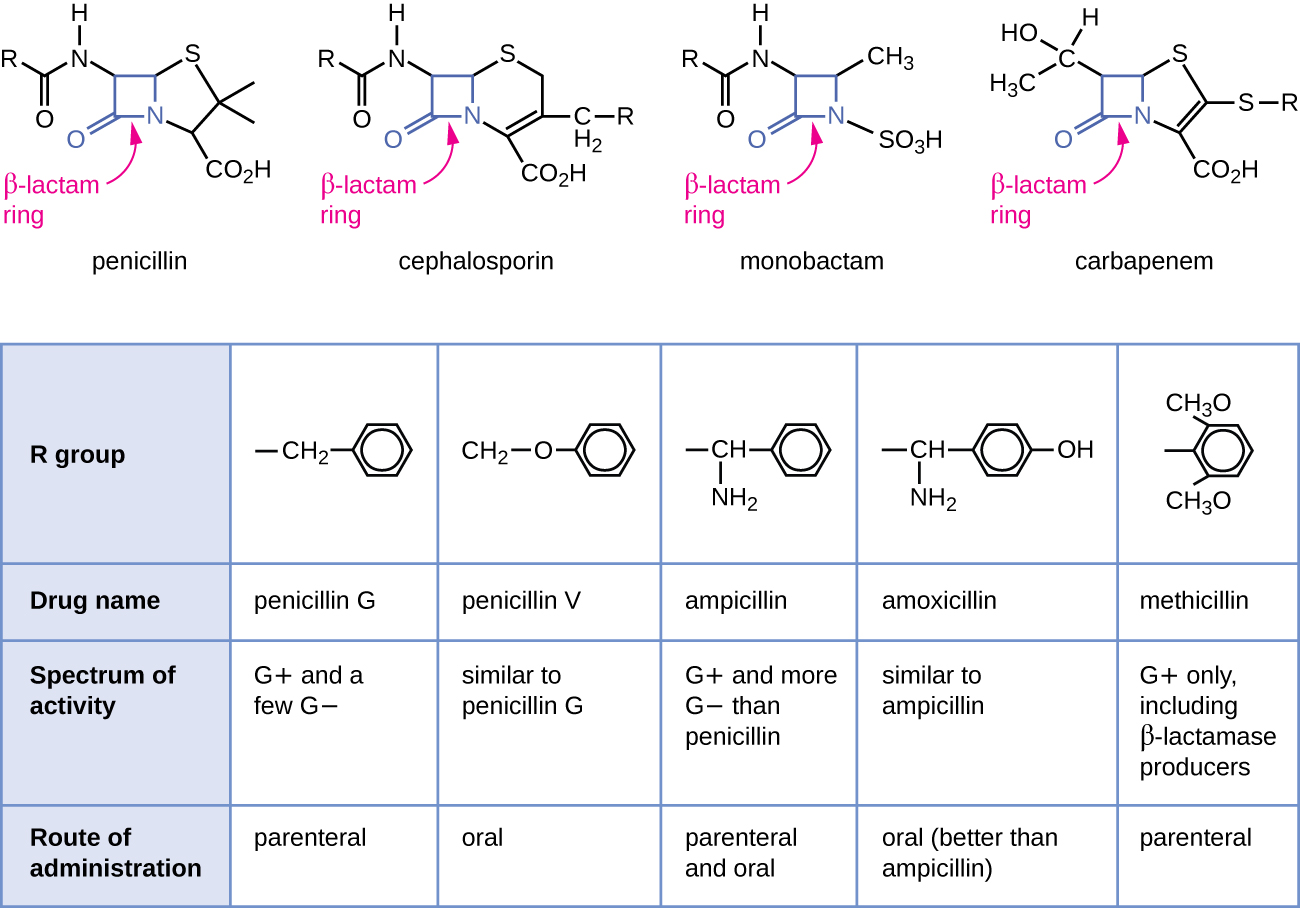
Cephalosporins are a slightly modified chemical "twin" to penicillins due to their beta lactam chemical structure. (See Figure 3.8 for a comparison of the beta-lactam ring structure, spectrum of activity, and route of administration across different classes of medications.) Because of these similarities, some patients who have allergies to penicillins may experience cross-sensitivity to cephalosporins.
Indications: Cephalosporins are used to treat skin and skin-structure infections, bone infections, genitourinary infections, otitis media, and community-acquired respiratory tract infections.
Mechanism of Action: Cephalosporins are typically bactericidal and are similar to penicillin in their action within the cell wall. Cephalosporins are sometimes grouped into "generations" by their antimicrobial properties. The 1st-generation drugs are effective mainly against gram-positive organisms. Higher generations generally have expanded spectra against aerobic gram-negative bacilli. The 5th-generation cephalosporins are active against methicillin-resistant Staphylococcus aureus (MRSA) or other complicated infections. [7]
Specific Administration Considerations: Patients who are allergic to pencillins may also be allergic to cephalosporins. Patients who consume cephalosporins while drinking alcoholic beverages may experience disulfiram-like reactions including severe headache, flushing, nausea, vomiting, etc.[8] Additionally, like penicillins, cephalosporins may interfere with coagulability and increase a patient's risk of bleeding. Cephalosporin dosing may require adjustment for patients experiencing renal impairment. Blood urea nitrogen (BUN) and creatinine should be monitored carefully to identify signs of nephrotoxicity.
Patient Teaching & Education: Patients who are prescribed cephalosporins should be specifically cautioned about a disulfiram reaction, which can occur when alcohol is ingested while taking the medication. Additionally, individuals should be instructed to monitor for rash and signs of superinfection (such as black, furry overgrowth on tongue; vaginal itching or discharge; loose or foul-smelling stool) and report to the prescribing provider.
It is also important to note that cephalosporin can enter breastmilk and may alter bowel flora of the infant. Thus, use during breastfeeding is often discouraged.[9]
Now let's take a closer look at the cephalosporin medication grid in Table 3.6.[10]
Table 3.6 Cephalosporin Medication Grid
Class/Subclass |
Prototype/Generics |
Administration Considerations |
Therapeutic Effects |
Side/Adverse Effects |
|---|---|---|---|---|
| Cephalosporins | 1st generation:
2nd generation: 3rd generation: 4th generation: 5th generation: |
Check for allergies, including if allergic to penicillin
Dosage adjustment if renal impairment Use with caution with seizure disorder PO: Administer without regard to food; if GI distress, give with food IV: Reconstitute drug with sterile water or normal saline; shake well until dissolved. Inject into large vein or free-flowing IV solution over 3-5 minutes Drug interaction: anticoagulants |
Monitor for systemic signs of infection:
-WBCs - Fever Monitor actual site of infection Monitor culture results, if obtained |
Common side effects:
-Nausea -Vomiting -Epigastric distress -Diarrhea Monitor for: -Rash -C-diff Nephrotoxicity if pre-existing renal disease Elevated INR and bleeding risk Development of hemolytic anemia |
Critical Thinking Activity 3.6a
Using the above grid information, consider the following clinical scenario question:
Mrs. Jenkins is an 89-year-old patient admitted to the medical surgical floor for treatment of a skin infection. The admitting provider prescribes Cefazolin 1 gram every 8 hours IV.
Mrs. Jenkins' admission laboratory tests include renal laboratory studies reflecting:
Creatinine: 1.3 mg/dL (Normal range: 1.2 mg/dL[11]
Blood urea nitrogen (BUN): 25 mg/dL (Normal: 8-20 mg/dL)
Glomerular Filtration Rate: 55 ml/min (Normal: 90-120 ml/min)[12]
On Day 3 Mrs. Jenkins has renal laboratory studies performed again. The results are:
Creatinine: 1.6 mg/dL
Blood urea nitrogen (BUN): 57 mg/dL
Glomerular Filtration Rate: 20 ml/min
Are Day 3 findings expected or not? What course of action should the nurse take?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
