1.3 Absorption
The first stage of pharmacokinetics is known as absorption. Absorption occurs after drugs enter the body and travel from the site of administration into the body’s circulation. Medications can enter the body through various routes of administration. Common routes to administer medications include the following examples:
- oral (swallowing an aspirin tablet)
- enteral (administering to the GI tract such as via a NG tube)
- rectal (administering an acetaminophen [Tylenol] suppository)
- inhalation (breathing in medication from an inhaler)
- intramuscular (getting a flu shot in the deltoid muscle)
- subcutaneous (injecting insulin into the fat tissue beneath the skin)
- transdermal (wearing a nicotine patch)
When a medication is administered orally or enterally, it faces its biggest hurdle during absorption in the gastrointestinal (GI) tract. Medications made of protein that are swallowed or otherwise absorbed in the GI tract may quickly be deactivated by enzymes as they pass through the stomach and duodenum. If the drug does get into the blood from the intestines, part of it will be broken down by liver enzymes, known as the first pass effect, and some of it will escape to the general circulation to either become protein-bound (inactive) or stay free (and create an action at a receptor site). These metabolic effects are further described in the “Metabolism” section later in this chapter. Thus, providers who prescribe medications, as well as nurses, understand that several doses of an oral medication may be needed before enough free drug stays active in the circulation to exert the desired effect.
What to do?
A workaround to the first pass effect is to administer the medication using alternate routes such as dermal, nasal, inhalation, injection, or intravenous. Alternative routes of medication administration bypass the first pass effect by entering the bloodstream directly or via absorption through the skin or lungs. Medications that are administered directly into the bloodstream (referred to as intravenous medications) do not undergo absorption and are fully available for distribution to tissues within the body.
Alternative routes of medication have other potential problems to consider. For example, injections are often painful and cause a break in the skin, an important barrier to infection. They can also be costly and difficult to administer daily, may cause localized side effects, or contribute to unpredictable fluctuations in medication blood levels.

Transdermal application of medication is an alternate route that has the primary benefit of slow, steady drug delivery directly to the bloodstream—without passing through the liver first. (See Figure 1.2[1] for an image of applying a transdermal patch.) Drugs delivered transdermally enter the blood via a meshwork of small arteries, veins, and capillaries in the skin. This makes the transdermal route of drug delivery particularly useful when a medication must be administered over a long period of time to control symptoms. For example, transdermal application of fentanyl, a pain medication, can provide effective pain management over a long period of time; the scopalamine patch can control motion sickness over the duration of a cruise ship vacation; and the nitroglycerin patch is used to control chronic chest pain. Despite their advantages, skin patches have a significant drawback in that only very small drug molecules can enter the body through the skin, making this application route not applicable for all types of medications.
Inhaling drugs through the nose or mouth is another alternative route for rapid medication delivery that bypasses the liver (see Figure 1.3).[2]) Metered-dose inhalers have been a mainstay of asthma therapy for several years, and nasal steroid medications are often prescribed for allergy and sinus problems.

Emerging discoveries & recent developments
Researchers are currently exploring alternative methods of drug delivery such as the use of inhaled insulin powders. Afrezza® is an example of an inhaled insulin approved by the Food and Drug Administration (FDA) to assist with blood sugar control. This technology stems from novel uses of chemistry and engineering to manufacture insulin particles of just the right size for absorption. If too large, the insulin particles could lodge in the lungs; if too small, the particles will be exhaled.[3]
Lifespan Considerations
Neonate & Pediatric: Gastric absorption in neonate and pediatric patients varies from that of their adult counterparts. In neonate and pediatric patients, the acid-producing cells of the stomach are immature until around the age of one to two years. Additionally, gastric emptying may be decreased because of slowed or irregular peristalsis (forward bowel movement). The liver of a neonatal or pediatric patient continues to mature, experiencing a decrease in first-pass elimination, resulting in higher drug levels in the bloodstream.[4]
Older Adult: As a natural result of aging, older adults will experience decreased blood flow to tissues within the GI tract. In addition, there may be changes in the gastric (stomach) pH that may alter the absorption of certain medications. Older adult patients may also experience variations in available plasma proteins, which can impact drug levels of medications that are highly protein-bound. Consideration must also be given to the use of subcutaneous and intramuscular injections in older patients experiencing decreased cardiac output. Decreased drug absorption of medications can occur when peripheral circulation is decreased. Finally, as adults age, they often have less body fat, resulting in decreased absorption of medication from transdermal patches that require adequate subcutaneous fat stores for proper absorption.[5]
Table 1 summarizes route considerations that a nurse should consider when administering medication.
Table 1. Route Considerations
Oral (PO) or Enteral (NGT, GT, OGT) Ingestion
- Oral route is a convenient route for administration of solid as well as liquid formulations.
- Additional variables that may influence the rate and extent of absorption include enteric coating or extended-release formulations, acidity of gastric contents, gastric emptying rate, dietary contents, and presence of other drugs.
- First pass effect: Blood containing the absorbed drug passes through the liver, which can deactivate a substantial amount of the drug and decrease its bioavailability (the percentage of dose that reaches the systemic circulation).
Parenteral Injection
- Subcutaneous and intramuscular administration: Injections can be difficult for patients to self-administer at home or to administer on a daily basis. They can be costly and painful. Injections also cause a break in skin that is an important barrier to infection, can cause fluctuation in drug levels. and can cause localized side effects to skin.
- Intravenous (IV): IV drugs are fully available to tissues after administration into the bloodstream, offering complete bioavailability and an immediate effect. However, this route requires intravenous access that can be painful to the patient and also increases risk for infection. Medications must be administered in sterile fashion, and if two products are administered simultaneously, their compatibility must be verified. There is also an increased risk of toxicity.
Pulmonary Inhalation
- Inhalation allows for rapid absorption of drugs in gaseous, vaporized, or aerosol form.
- Absorption of particulates/aerosols depends on particle/droplet size, which influences depth of entry through the pulmonary tree to reach the alveoli.
- The ability of the patient to create successful inhalation, especially in the presence of bronchospasm, may also influence depth of entry in the pulmonary tree.
Topical and Transdermal Application
- Topical creams, lotions, and ointments are generally used for local effect; transdermal patch formulations are used for systemic effect.
- Absorption through the buccal or sublingual membranes may be rapid.
- Absorption through skin is generally slower but produces steady, long-term effect that avoids the first pass effect. However, absorption of medication is affected by blood flow to the skin. [6]
Interactive Activity
- "Applying transdermal patch.jpg" by British Columbia Institute of Technology (BCIT) is licensed under CC BY 4.0 ↵
- “Adult Using Asthma Inhaler” by NIAID is licensed under CC BY 2.0 ↵
- This work is a derivative of Medicines by Design by US Department of Health and Human Services, National Institute of Health, National Institute of General Medical Sciences and is available in the public domain. ↵
- Fernandez, E., Perez, R., Hernandez, A., Tejada, P., Arteta, M., & Ramos, J. T. (2011). Factors and mechanisms for pharmacokinetic differences between pediatric population and adults. Pharmaceutics, 3(1), 53–72. https://doi.org/10.3390/pharmaceutics3010053 ↵
- Fernandez, E., Perez, R., Hernandez, A., Tejada, P., Arteta, M., & Ramos, J. T. (2011). Factors and mechanisms for pharmacokinetic differences between pediatric population and adults. Pharmaceutics, 3(1), 53–72. https://doi.org/10.3390/pharmaceutics3010053 ↵
- This work is a derivative of Principles of Pharmacology by LibreTexts licensed under CC BY-NC-SA 4.0. ↵
Basic Concepts Related to Antimicrobial Therapy
Before we learn about medications that are used to treat infections in our patients, we must first understand the basics of microbiology. Let's begin with a review of bacteria. Bacteria are found in nearly every habitat on earth, including within and on humans. Most bacteria are harmless or considered helpful, but some are pathogens. A pathogen is defined as an organism causing disease to its host. Pathogens, when overgrown, can cause significant health problems or even death for your patients.
Bacteria may be identified when a patient has an infection by using a culture and sensitivity test or a gram stain test. Antimicrobials may be classified as broad-spectrum or narrow-spectrum, based on the variety of bacteria they effectively treat. Additionally, antibiotics may be bacteriostatic or bactericidal in terms of how it targets the bacteria. Finally, the mechanism of action is also considered in the selection of an antibiotic.
In addition to antibiotics, antimicrobials also include medications used to treat viruses and fungi. Each of these topics will be discussed in more detail below, along with the issue of drug resistance.
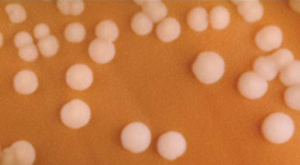
Culture and Sensitivity
When a patient presents signs or symptoms of an infection, healthcare providers will begin the detective work needed to identify the source of the infection. A culture is a test performed to examine different body substances for the presence of bacteria or fungus.[1] These culture samples are commonly collected from a patient's blood, urine, sputum, wound bed, etc. Nurses are commonly responsible for the collection of culture samples and must be conscientious to collect the sample prior to the administration of antibiotics. Antibiotic administration prior to a culture can result in a delayed identification of the organism and complicate the patient's recovery. Once culture samples are collected, they are then incubated in a solution that promotes bacterial or fungal growth and spread onto a special culture plate.[2] Clinical microbiologists subsequently monitor the culture for signs of organism growth to aid in the diagnosis of the infectious pathogen. A sensitivity analysis is often performed to select an effective antibiotic to treat the microorganism. If the organism shows resistance to the antibiotics used in the test, those antibiotics will not provide effective treatment for the patient's infection. Sometimes a patient may begin antibiotic treatment for an infection, but will be switched to a different, more effective antibiotic based on the culture and sensitivity results.[3]
Gram Positive vs. Gram Negative
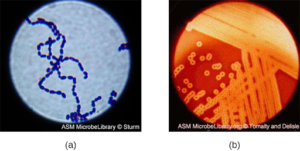
A gram stain is another type of test that is used to assist in classification of pathogens. Gram stains are useful for quickly identifying if bacteria are "gram positive" or "gram negative," based on the staining patterns of their cellular walls. Utilizing gram stain allows microbiologists to look for characteristic violet (Gram +) or red/pink (Gram -) staining patterns when they examine the organisms under a microscope.[4] Identification of bacteria as gram positive or gram negative assists the healthcare provider in quickly selecting an appropriate antibiotic to treat the infection.
Sample Gram Positive Infections
Streptococcus, the name which comes from the Greek word for twisted chain, is responsible for many types of infectious diseases in humans. Streptococcus is an example of a Gram + infection and is identified by its ability to lyse, or breakdown, red blood cells when grown on blood agar.
S. pyogenes is a type of β-hemolytic Streptococcus. This species is considered a pyogenic pathogen because of the associated pus production observed with infections it causes (see Figure 3.1[5] for an image of Streptococcus undergoing gram staining). S. pyogenes is the most common cause of bacterial pharyngitis (strep throat); it is also a common cause of various skin infections that can be relatively mild (e.g., impetigo) or life threatening (e.g., necrotizing fasciitis, also known as flesh-eating disease).[6]

Staphylococcus is a second example of a Gram + bacteria. The bacteria Staphylococcus comes from a Greek word for bunches of grapes, which describes their microscopic appearance in culture. Strains of S. aureus cause a wide variety of infections in humans, including skin infections that produce boils, carbuncles, cellulitis, or impetigo. Many strains of S. aureus have developed resistance to antibiotics. Some antibiotic-resistant strains are designated as methicillin-resistant S. aureus (MRSA) and vancomycin-resistant S. aureus (VRSA) . These strains are some of the most difficult to treat because they exhibit resistance to nearly all available antibiotics, not just methicillin and vancomycin. Because they are difficult to treat with antibiotics, infections can be lethal. MRSA and VRSA are also contagious, posing a serious threat in hospitals, nursing homes, dialysis facilities, and other places where there are large populations of elderly, bedridden, and/or immunocompromised patients.[7] See Figure 3.2[8] for an image of Staphylococcus bacteria microscopically.
Sample Gram Negative Infections
Gram negative bacteria often grow between aerobic and anaerobic areas (such as in the intestines). Some gram negative bacteria cause severe, sometimes life-threatening disease. The genus Neisseria, for example, includes the bacteria N. gonorrhoeae, the causative agent of the sexually transmitted infection gonorrhea, and N. meningitides, the causative agent of bacterial meningitis. See Figure 3.3[9] for an image of Neisseria meningitides. Another common gram negative infection that is seen in hospitalized patients is Escherichia coli (E. Coli). This is a frequent culprit for urinary tract infections due to its presence in the GI tract.
Broad-Spectrum vs. Narrow-Spectrum Antimicrobials
Spectrum of activity is one of the factors that providers use when selecting antibiotics to treat a patient's infection. A narrow-spectrum antimicrobial targets only specific subsets of bacterial pathogens.[10] For example, some narrow-spectrum drugs only target gram positive bacteria, but others target only gram negative bacteria. If the pathogen causing infection has been identified in a culture and sensitivity test, it is best to use a narrow-spectrum antimicrobial and minimize collateral damage to the normal microbacteria.
A broad-spectrum antimicrobial targets a wide variety of bacterial pathogens, including both gram positive and gram negative species, and is frequently used to cover a wide range of potential pathogens while waiting on the laboratory identification of the infecting pathogen. Broad-spectrum antimicrobials are also used for polymicrobial infections (a mixed infection with multiple bacterial species) or as prophylactic prevention of infections with surgery/invasive procedures. Finally, broad-spectrum antimicrobials may be selected to treat an infection when a narrow-spectrum drug fails because of development of drug resistance by the target pathogen.[11]
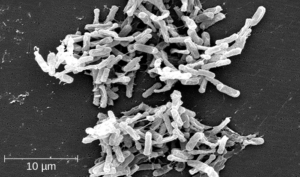
One risk associated with using broad-spectrum antimicrobials is that they will also target a broad spectrum of the normal microbacteria that can cause diarrhea. They also increase the risk of a superinfection , a secondary infection in a patient having a preexisting infection. A superinfection develops when the antibacterial intended for the preexisting infection kills the protective microbiota, allowing another pathogen resistant to the antibacterial to proliferate and cause a secondary infection. Common examples of superinfections that develop as a result of antimicrobial use include yeast infections (candidiasis) and pseudomembranous colitis caused by Clostridium difficile (C-diff), which can be fatal.[12] Probiotics, such as lactobacillus, are commonly used for individuals with C-diff to introduce normal bacteria into the gastrointestinal system and improve bowel function. See Figure 3.4[13] for an image of C-diff microscopically.
Let's recap…
- A broad-spectrum antibiotic will treat gram positive and gram negative bacteria.
- A narrow-spectrum antibiotic will treat either gram positive or gram negative bacteria.
If a patient is started on an antibiotic that is gram + and the culture identifies a gram - organism, the medication will not improve the patient's status. The selection of an incorrect antibiotic can lead to adverse reactions and increase bacterial resistance.
At times, a broad spectrum antibiotic may be administered prior to receiving the culture report due to the severity of the illness of the patient. Once the culture is reported, the antibiotic therapy is tailored to the patient. It is the nurse's responsibility to review culture results and ensure that the results have been communicated to the prescribing provider.
Antibacterials Actions -- Bacteriostatic vs. Bactericidal
When a provider selects an antibacterial drug, it is important to consider how and where the drug will ultimately target the bacteria. Antibacterial drugs can be either bacteriostatic or bactericidal in their interactions with the offending bacteria. Bacteriostatic drugs cause bacteria to stop reproducing; however, they may not ultimately kill the bacteria. In contrast, bactericidal drugs kill their target bacteria.
The decision about whether to use a bacteriostatic or bactericidal drug often depends on the type of infection and the overall immune status of the patient. In a healthy patient with strong immune defenses, both bacteriostatic and bactericidal drugs can be effective in achieving clinical cure. However, when a patient is immunocompromised, a bactericidal drug is essential for the successful treatment of infections. Regardless of the immune status of the patient, life-threatening infections such as acute endocarditis require the use of a bactericidal drug to eliminate all offending bacteria.[14]
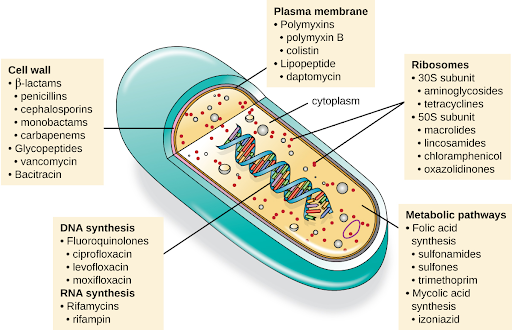
Mechanism of Action
Another consideration in the selection of an antibacterial drug is the drug's mechanism of action. Each class of antibacterial drugs has a unique mechanism of action , the way in which a drug affects microbes at the cellular level. For example, cephalosporins act on the integrity of the cell wall. In contrast, aminoglycosides impact ribosome function and inhibit protein synthesis, which stops the proliferation of cells.[15] See Figure 3.5[16] for a summary of how various antibiotics affect the cell wall, the plasma membrane, the ribosomes, the metabolic pathways, or DNA synthesis of bacteria.
Antiviral
Similar to antibacterial medications, antiviral drugs directly impact interaction and reproduction of the offending microorganism. Antibacterial medications are required for treating bacterial infections; antivirals treat specific viral infections. For example, oseltamivir (Tamiflu) is commonly prescribed to treat influenza. Unlike antimicrobials, antiviral medications do not kill the offending virus, but they work to reduce replication and development of the virus.[17]
Antifungal
Antifungal, or antimycotic agents, are medications that are used to treat fungal infections. These medications work by killing the cells of the fungus or inhibiting the reproduction of the cells. Unlike antibacterial and antiviral medications, many antifungals are applied topically to the affected area. Fungal infections commonly affect surface areas of the body, including the toes, nails, mouth, groin, etc. For example, Candida albicans is a type of fungi that when overgrown in the mouth produces oral thrush. Patients experiencing thrush may be prescribed oral antifungal swish and spit medication such as nystatin.
Drug Resistance
Although there is a wide availability of medications that are useful for treating infection, greater limitations in effectiveness are being seen. According to the Centers for Disease Control (2019), each year in the United States, at least 2 million people are infected with an antibiotic-resistant infection, and more than 23,000 die.[18]
Prevention Strategies
In the United States and many other countries, most antimicrobial drugs are self-administered by patients at home. Unfortunately, many patients stop taking antimicrobials once their symptoms dissipate and they feel better. If a 10-day course of treatment is prescribed, many patients only take the drug for 5 or 6 days, unaware of the negative consequences of not completing the full course of treatment.
The Problem: A shorter course of treatment not only fails to kill the target organisms to the expected levels but also assists in creating drug-resistant variants within the body. A patient's nonadherence amplifies drug resistance when the recommended course of treatment is long.
For example, treatment for tuberculosis (TB) has a recommended treatment regimen lasting from 6 months to a year. The CDC estimates that about one third of the world's population is infected with TB, most living in underdeveloped or underserved regions where antimicrobial drugs are available over the counter. In such countries, there may be even lower rates of adherence than in developed areas. Nonadherence leads to antibiotic resistance and more difficulty in controlling pathogens. As a direct result, the emergence of multidrug-resistant strains of TB is becoming a huge problem.
The over prescription of antimicrobials also contributes to antibiotic resistance. Patients often demand antibiotics for diseases that do not require them, like viral colds and ear infections. Pharmaceutical companies aggressively market drugs to physicians and clinics, making it easy for them to give free samples to patients, and some pharmacies even offer certain antibiotics free to low-income patients with a prescription.
In recent years, various initiatives have aimed to educate parents and clinicians about the judicious use of antibiotics. However, previous studies have shown the parental expectations for antimicrobial prescriptions for children actually increased.
One possible solution that is being explored is a regimen called directly observed therapy (DOT), which involves the supervised administration of medications to patients. Patients are either required to visit a health-care facility to receive their medications, or health-care professionals must administer medication in patients' homes or another designated location. DOT has been implemented in many cases for the treatment of TB and has been shown to be effective; indeed, DOT is an integral part of WHO's global strategy for eradicating TB.
But is this a practical strategy for all antibiotics? Would patients taking penicillin, for example, be more or less likely to adhere to the full course of treatment if they had to travel to a health-care facility to receive each dose? Who would pay for the increased cost associated with DOT? When it comes to overprescription, should providers or drug companies be policed when it comes to over prescribing antibiotics to enforce best practices? What group should assume this responsibility, and what penalties would be effective in discouraging overprescription?
This is a complex issue with no clear, easy solution. However, what is clear is that all patients need extensive education regarding the judicious and complete use of medications to increase adherence and decrease the opportunity for antimicrobial resistance.[19]
Critical Thinking Activity 3.2a
Reflecting on current healthcare challenges regarding the ongoing emergence of antimicrobial resistant organisms, what actions could you take within your nursing practice to help prevent drug resistance?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
