1.7 Pharmacodynamics
Complex Interactions
So far, we have learned the importance of pharmacokinetics in describing how the body absorbs, moves, processes, and eliminates a medication. Now let’s consider a drug’s impact on the body, a series of complex interactions known as pharmacodynamics.
When considering how the cells of the body respond to medications, it is important to remember that the majority of drugs bind to specific receptors on the surface or interior of cells. However, there are many other cellular components and non-specific sites that can serve as receptor sites where drugs can bind to create a response. For example, did you know that an osmotic laxative like magnesium citrate attracts and binds with water? This medication works to pull water content into the bowel and increases the likelihood of a bowel movement.
Other medications may inhibit specific enzyme binding sites in order to impact the functionality of a cell or tissue. For example, antimicrobial and antineoplastic drugs commonly work by inhibiting enzymes that are critical to the function of the cell. With blockage of the enzyme binding site, the cell microbe or neoplastic cell is no longer viable and cell death occurs.
Agonist and Antagonist Actions
Understanding the mechanism of action,[1] or how a medication functions within the body, is essential to understanding the processes medications go through to produce the desired effect (see Figure 1.6). Drugs have agonistic or antagonistic effects. A drug agonist binds tightly to a receptor to produce a desired effect. A drug antagonist competes with other molecules and blocks a specific action or response at a receptor site. For example, the cardiac medication atenolol (Tenormin) is a beta-1 receptor antagonist used to treat patients with hypertension or heart disease. Beta-1 receptor antagonist medications like atenolol produce several effects by blocking beta-1 receptors: a negative inotropic effect occurs by weakening the contraction of the heart, thus causing less work of the heart muscle; a negative chronotropic effect occurs when the heart rate is decreased; and a negative dromotropic effect occurs when the conduction of the electrical charge in the heart is slowed. Understanding the effects of a beta-1 antagonist medication allows the nurse to anticipate expected actions of the medication and the patient response. Agonistic and antagonistic effects on receptors are further discussed in the “Autonomic Nervous System” chapter. [2]
Critical Thinking Activity 1.7a
Atenolol (Tenormin) is a beta-1 antagonist with a negative inotropic and chronotropic effects. What should a nurse assess before administration?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” sections at the end of the book.
- "Mechanism of Action" by Dominic Slausen at Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- This work is a derivative of Principles of Pharmacology by LibreTexts licensed under CC BY-NC-SA 4.0. ↵
Lightbulb Moment
Let's apply what you have learned in the respiratory unit.
Asthma Scenario
An adult patient presents to the emergency department with complaints of shortness of breath and increased work of breathing. The patient is alert and oriented times 3, skin is pink, warm and dry, BP 148/88, T 98, P92, R 24, pulse oximetry 91% on room air. Assessment of the lung reveals expiratory wheezing throughout the lung fields. The patient has a past medical history of asthma, hypertension, and diabetes.
- The nurse anticipates which of the following medications will be initially administered to the patient?
a) Theophylline
b) Montelukast
c) Albuterol
d) Salmeterol
2. List the steps the nurse should take to safely administer the medication.
3. What assessments should the nurse plan to complete after administering the medication?
4. The nurse plans on teaching the patient about using the albuterol inhaler at home. What information should be included?
5. What is the best method for the nurse to use to ensure that the patient is correctly using an inhaler?
Allergy Scenario
A pediatric patient presents to the emergency department with complaints of shortness of breath, increased work of breathing, and a cough. The patient is alert and oriented times 3, skin is pink, warm and dry, BP 112/68, T 99, P106, R 32, pulse oximetry 90% on room air. Assessment of the lung sounds reveals diminished lung sounds throughout all lung fields. The patient has a past medical history of peanut allergy. The mother tells you that they were at a birthday party and after consumption of a cupcake, the symptoms started.
6. The nurse anticipates that which of the following medication will be likely ordered for this patient?
a. Diphenhydramine
b. Epinephrine
c. Cetirizine
d. Guaifenesin
Note: Answers to the Lightbulb Moment can be found in the "Answer Key" sections at the end of the book.
Interactive Activity
Interactive Activity
Interactive Activity
Attributions:
- “301317.png” by oksmith is in the public domain
- “Learning-3245793_960_720.jpg” by harishs is licensed under CC0
- “Asthma-MA.jpg” by ARISE Project is licensed under CC BY 4.0
- Open RN Project. (2020, January 14). Clinic handoff video captioned 0153. [Video]. YouTube. Licensed under CC BY 4.0. https://youtu.be/VsiQ6s_deiw
- Open RN Project. (2020, January 14). Patient video captioned 0156. [Video]. YouTube. Licensed under CC BY 4.0. https://youtu.be/EE7Jifu5T-w
- “Stethoscope-2.png” by Sonarpulse is in the public domain
- “Posterior Left Lower Lung - 00329.JPG” by ARISE Project is licensed under CC BY 4.0
- “Posterior Right Upper Lung - 00328.JPG” by ARISE Project is licensed under CC BY 4.0
- “Ehr-1476525_960_720.png” by mcmurryjulie is licensed under CC0
- “Peak Flow - 2047.JPG” by ARISE Project is licensed under CC BY 4.0 - need link
- Open RN Project. (2020, January 14). Inhaler initial. [Video]. YouTube. Licensed under CC BY 4.0. https://youtu.be/KY-jSi_vbBQ
- Open RN Project. (2020, January 14). Inhaler with spacer. [Video]. YouTube. Licensed under CC BY 4.0. https://youtu.be/WhOzMLV6_p4
- “Doctor_Talking_on_the_Phone_Cartoon.svg from Wikimedia Commons” by VideoPlasty.com is licensed under CC BY-SA 4.0“A_Businessman_Holding_A_Thank_You_Sign.svg” by FriendlyStock.com is licensed under CC
Now that we have reviewed antimicrobial basics and administration considerations, we will take a closer look at specific antimicrobial classes and administration considerations, therapeutic effects, adverse effects, and specific teaching needed for each class of antimicrobials. But before we do that, let's reexamine the importance of the nursing process in guiding the nurse who administers antimicrobial medications. The nursing process consists of assessment, diagnosis, outcome identification, planning, implementation of interventions, and evaluation. For more information about the nursing process, refer to the Chapter 2 sub-module on "Ethical and Professional Foundations of Safe Medication Administration by Nurses." Because diagnosis, outcome identification, and planning are specifically tailored to the individual patient, we will broadly discuss considerations related to assessment, implementation of interventions, and evaluation when administering antimicrobials.
Nursing Process: Assessment
Although there are numerous details to consider when administering medications, it is important to always first think more broadly about what you are giving and why. As a nurse who is administering an antimicrobial, you must remember some important broad considerations.
First, let's think of the WHY?
Antimicrobials are given to prevent or treat infection. If a patient is prescribed an antimicrobial, an important piece of the nursing assessment should be to look for signs and symptoms of infection. The nurse should always know WHY the patient is receiving an antimicrobial to evaluate if the patient is improving or deteriorating. Remember, the nurse must assess how this medication is working, and having pre-administration assessment information is an important part of this process. Typical data that a nurse collects at the start of a shift include a baseline temperature, heart rate, blood pressure, and white blood cell count. Focused assessments are then made based on the type of infection. For example, if it is a wound infection, the wound should be assessed. If it is a respiratory infection, the nurse should assess the patient's lung sounds. If a patient has a urinary tract infection (UTI), the urine and symptoms related to a UTI should be assessed. Additionally, whenever a patient has an infection, it is important to continually monitor for the development of sepsis, a life-threatening condition caused by severe infection. Early signs of sepsis include new onset confusion, elevated heart rate, decreased blood pressure, increased respiratory rate, and elevated fever.
Additional baseline information to collect prior to the administration of any new medication order includes a patient history, current medication use including herbals or other supplements, and history of allergy or previous adverse response. Many patients with an allergy to one type of antimicrobial agent may experience cross-reactivity to other classes. This information should be appropriately communicated to the prescribing provider prior to the administration of any antimicrobial medication.
Nursing Process: Implementation of Interventions
With administration of the antimicrobial medication, it is important for the nurse to anticipate any additional interventions associated with the medications. For example, antimicrobials often cause gastrointestinal upset (GI) such as nausea, diarrhea, etc. The patient should be educated about these potential side effects, and proper interventions should be taken to minimize these occurrences. For example, the nurse may instruct the patient to take certain antimicrobials with food to diminish the chance of GI upset, whereas other medications should be taken on an empty stomach for optimal absorption.
Hypersensitivity/allergic reactions are always a potential adverse reaction, especially when administering the first dose of a new antibiotic, and the nurse should monitor for these symptoms closely and respond appropriately by immediately notifying the prescriber. Hypersensitivity reactions are immune responses that are exaggerated or inappropriate to an antigen and can range from itching to anaphylaxis. Anaphylaxis is a medical emergency that can cause life-threatening respiratory failure. Early signs of anaphylaxis include, but are not limited to, hives and itching, the feeling of a swollen tongue or throat, shortness of breath, dizziness, and low blood pressure.
Nursing Process: Evaluation
Finally, it is important to always evaluate the patient's response to a medication. With antimicrobial medications, the nurse should assess for absence of or decreasing signs of infection, indicating the patient is improving. It is important to document these findings to reflect the patient's trended response.
Additionally, it is also important for the nurse to promptly identify and communicate signs of worsening infection to the provider. For example, increasing white blood cell count, temperature, heart rate, and respiratory rate may indicate that the patient's body is experiencing a life-threatening response to the infection. These signs of worsening clinical assessment require prompt intervention to prevent further clinical deterioration. Additionally, patients receiving antibiotics should be closely monitored for developing a complication called "C-diff," resulting in frequent, foul-smelling stools. C-diff requires the implementation of modified contact precautions, including the use of soap and water, not hand sanitizer, as well as antibiotic therapy. [1]
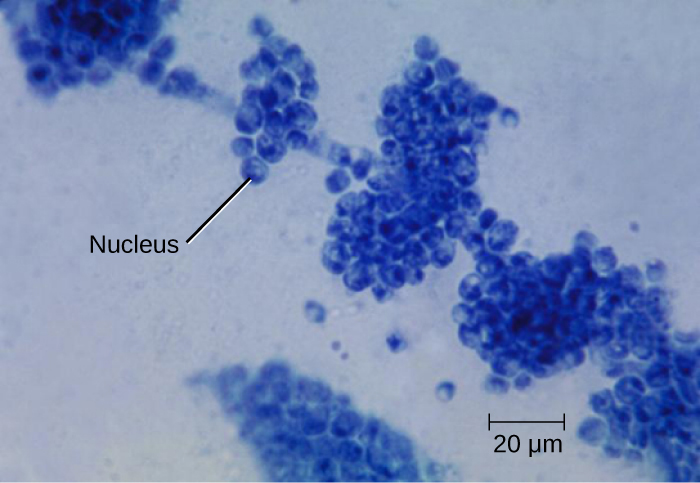
Fungi are important to humans in a variety of ways. Both microscopic and macroscopic fungi have medical relevance, but some pathogenic species that can cause mycoses (illnesses caused by fungi). See Figure 3.13 for a microscopic image of candida albicans that is the causative agent of yeast infections. Some pathogenic fungi are opportunistic, meaning that they mainly cause infections when the host's immune defenses are compromised and do not normally cause illness in healthy individuals. Fungi are important in other ways. They act as decomposers in the environment, and they are critical for the production of certain foods such as cheeses. Fungi are also major sources of antibiotics, such as penicillin from the fungus Penicillium.[3].
Indications:
Imidazoles are synthetic fungicides commonly used in medical applications and also in agriculture to keep seeds and harvested crops from molding. Examples include miconazole, ketoconazole, and clotrimazole, which are used to treat fungal skin infections such as ringworm, specifically tinea pedis (athlete's foot), tinea cruris (jock itch), and tinea corporis.
Triazole drugs, including fluconazole, can be administered orally or intravenously for the treatment of several types of systemic yeast infections, including oral thrush and cryptococcal meningitis, both of which are prevalent in patients with AIDS. Triazoles also exhibit more selective toxicity, compared with the imidazoles, and are associated with fewer side effects.[4]
Allylamines, a structurally different class of synthetic antifungal drugs, are most commonly used topically for the treatment of dermatophytic skin infections like athlete's foot, ringworm, and jock itch. Oral treatment with terbinafine is also used for fingernail and toenail fungus, but it can be associated with the rare side effect of hepatotoxicity.[5]
Polyenes are a class of antifungal agents naturally produced by certain actinomycete soil bacteria and are structurally related to macrolides. Common examples include nystatin and amphotericin B. Nystatin is typically used as a topical treatment for yeast infections of the skin, mouth, and vagina, but may also be used for intestinal fungal infections. The drug amphotericin B is used for systemic fungal infections like aspergillosis, cryptococcal meningitis, histoplasmosis, blastomycosis, and candidiasis. Amphotericin B was the only antifungal drug available for several decades, but its use has associated serious side effects, including nephrotoxicity.[6]
Mechanism of Action: Antifungals disrupt ergosterol biosyntheses of the cell membrane increasing cellular permeability and causing cell death.
Special Administration Considerations: Administration guidelines will vary depending on the type of fungal infection being treated. It is important to monitor response of the affected area and examine class specific administration considerations to monitor patient response.
Patient Teaching & Education: The patient should be advised to follow dosage instructions carefully and finish the drug completely, even if they feel their symptoms have resolved. The patient should report any skin rash, abdominal pain, fever, or diarrhea to the provider. The patient should monitor carefully for unexplained bruising or bleeding, which may be a sign of liver dysfunction.[7]
Now let's take a closer look at the medication grid for various antifungals in Table 3.15.[8]
Table 3.15 Antifungal Medication Grid
| Class/Subclass | Prototype/Generic | Administration Considerations | Therapeutic Effects | Side/Adverse Effects |
|---|---|---|---|---|
| Antifungals | clotrimazole | Check for allergies
Topical cream: apply liberally twice daily to affected area |
Improve symptoms of athlete's foot (tinea pedis), jock itch (tinea cruris), or ringworm | Topical-skin irritation, rash |
| fluconazole | Check for allergies
Route: PO/IV Single or multiple doses Caution if liver dysfunction Potential for fetal harm |
Improve symptoms of yeast infection | Hepatotoxicity | |
| terbinafine | Cream or aerosol
Wash affected area with soap and water and allow to dry completely before applying |
Improve symptoms of athlete's foot (tinea pedis), jock itch (tinea cruris), or ringworm | External use only | |
| nystatin | PO: If order is "'swish and swallow," instruct patient to hold medication in mouth for several minutes before swallowing
Topical cream/powder: apply liberally twice daily |
Improve symptoms of yeast infection of skin | External use only | |
| amphotericin B | Check for allergies
Route: IV Reconstitute and dilute as directed on packaging Administer slowly over several hours initially and monitor VS every 30 minutes; may require premedication Therapy may take several months Alert: Different amphotericin B preparations aren't interchangeable Caution if renal impairment Black Box Warning: Don't use to treat noninvasive forms of fungal disease in patients with normal neutrophil counts |
Improvement of systemic fungal infection such as aspergillis | Monitor fluid intake and output; report change in urine appearance or volume
Monitor BUN and creatinine levels two or three times weekly. Kidney damage may be reversible if drug is stopped at first sign of renal dysfunction Hydrate patient before infusion to reduce risk of nephrotoxicity Obtain liver function tests once or twice weekly Monitor CBC weekly Monitor potassium level closely and report signs of hypokalemia Check calcium and magnesium levels twice weekly Drug may be ototoxic. Report evidence of hearing loss, tinnitus, vertigo, or unsteady gait |
Critical Thinking Activity 3.15a
Using the above grid information, consider the following clinical scenario question:
A patient in a skilled nursing facility has been receiving nystatin applied to groin folds twice daily for several weeks, but there is no sign of improvement. What is the nurse's best response?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
