1.9 Examining Effect
Onset, Peak, and Duration
Dosing considerations play an important role in understanding the effect that a medication may have on a patient. During administration, the nurse must pay close attention to the desired effect and therapeutic patient response, as well as the safe dose range for any medication. The nurse should have an understanding of medication efficacy in order to ensure its appropriateness. If a nurse is provided different medication choices according to a provider’s written protocol, the nurse should select the option with the anticipated desired therapeutic response. Additionally, the nurse must be aware of the overall dose-response based on the dosage selected.
Three additional principles related to the effect of a medication on a patient are onset, peak, and duration.
Onset: the onset of medication refers to when the medication first begins to take effect
Peak : the peak of medication refers to the maximum concentration of medication in the body, and the patient shows evidence of greatest therapeutic effect
Duration: the duration of medication refers to the length of time the medication produces its desired therapeutic effect
Consider this patient care example and apply the principles of onset, peak, and duration: A 67-year-old female post-operative patient rings the call light to request medication for pain related to the hip replacement procedure she had earlier that day. She notes her pain is “excruciating, a definite 9 out of 10.” Her brow is furrowed, and she is grimacing in obvious discomfort. As the nurse providing care for the patient, you examine her post-operative medication orders and consider the pain medication options available to you. In reviewing the various options, it is important to consider how quickly a medication will work (onset), when the medication will reach maximum effectiveness (peak), and how long the pain relief will last (duration). Understanding these principles is important in effectively relieving the patient’s pain and constructing an overall plan of care.
Critical Thinking Activities 1.9
- At 0500, your patient who had a total knee replacement yesterday rates his pain while walking as 7 out of 10. Physical therapy is scheduled at 0900. The patient has acetaminophen (Tylenol) 625 mg ordered every four hours as needed for discomfort. What should you consider in relation to the administration and timing of the patient’s pain medication?
2. Your patient is prescribed NPH insulin to be given at breakfast and supper. As a student nurse, you know that insulin is used to decrease blood sugar levels in patients with diabetes mellitus. During report, you hear that the patient has been ill with GI upset during the night, and the nursing assistant just informed you he refused his breakfast tray. While reviewing this medication order, you consider the purpose of the medication and information related to the medication’s onset, peak, and duration. When reviewing the drug reference, you find the NPH insulin has an onset of about 1 – 3 hours after medication administration. What should you consider in relation to the administration and timing of the patient’s insulin?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” sections at the end of the book.
Duration and Dosing
Now let’s consider the implication of duration and dosing. Remember the duration of medication is correlated with the elimination. If a medication has a short half-life (and thus eliminated more quickly from the body), the therapeutic effect is shorter. These medications may require repeated dosing throughout the day in order to achieve steady blood levels of active free drug and a sustained therapeutic effect. Other medications have a longer half-life (and thus longer therapeutic duration) and are only given once or twice per day. For example, oxycondone immediate release is prescribed every 4 to 6 hours for the therapeutic effect of immediate relief of severe pain, whereas oxycodone ER (extended release) is prescribed every 12 hours for the therapeutic effect of sustained relief of severe pain.
Indications: Fluoroquinolones may be used to treat pneumonia or complicated skin or urinary tract infections.
Mechanism of Action: Fluoroquinolones are a synthetic antibacterial medication that work by inhibiting the bacterial DNA replication. They are bacteriocidal due to the action they take against the DNA of the bacterial cell wall. Many fluoroquinolones are broad spectrum and effective against a wide variety of both gram-positive and gram-negative bacteria.
Specific Administration Considerations: Patients taking oral fluoroquinolones should avoid the use of antacid medication as antacids significantly impede absorption. Patients should also be instructed to take oral fluoroquinolones with a full glass of water two hours before or after meals to enhance absorption and prevent crystalluria. Fluoroquinolone therapy is contraindicated in children except for complicated UTIs, pyelonephritis, plague, or post Anthrax exposure and should be used cautiously in pregnancy.[1]
Black Box Warning: Black Box Warnings are the strongest warnings issued by the Federal Drug Association (FDA) and signify that the medical studies have indicated that the drug carries a significant risk of serious or life-threatening adverse effects.
Fluoroquinolones, including levofloxacin, have been associated with disabling and potentially irreversible serious adverse reactions, including:
- Tendinitis and tendon rupture
- Peripheral neuropathy
- Central nervous system effects
- Exacerbation of muscle weakness in patients with myasthenia gravis
In patients who experience any of these serious adverse reactions, discontinue the medication immediately, and avoid the use of fluoroquinolones.
Patient Teaching & Education: All patients on fluoroquinolone therapy should be instructed to avoid direct and indirect sunlight due to the photosensitivity that can be experienced while on these medications. The patient should take measures to ensure that dosages are spaced evenly throughout the day and that fluid balance is maintained. It is important to maintain an intake of 1500mL-2000mL per day while taking the medication. The patient should be advised that medications containing calcium, aluminum, iron, or zinc may impair absorption and should be avoided. Other side effects of fluoroquinolones increase drowsiness. Additionally, the patient should be cautioned to monitor for episodes of fainting or decreased heart rate and report any history of prolonged QT syndrome. If a patient notices peripheral neuropathy occurring, this should be reported to the healthcare provider. Additional side effects to monitor include increased tendon pain, jaundice, rash, or mood changes.[2]
Now let's take a closer look at the medication grid for levofloxacin in Table 3.10.[3]
Table 3.10 Fluoroquinolone Medication Grid
Class/Subclass |
Prototype/Generic |
Administration Considerations |
Therapeutic Effects |
Side/Adverse Effects |
|---|---|---|---|---|
| Fluoroquinolones | levofloxacin | Check for allergies
Give with plenty of fluids Oral: Administer 2 hours before or after meals, antacid, or iron IV: Infuse 500 mg or less over 60 minutes and doses of 750 mg over 90 minutes Dosage adjustment if renal or hepatic impairment Use cautiously if history of seizures |
Monitor for systemic signs of infection:
-WBCs -Fever Monitor actual site of infection Monitor culture results, if obtained |
Discontinue immediately if tendonitis, tendon rupture, peripheral neuropathy, CNS effects, or muscle weakness in patients with Myasthenia Gravis
Monitor for: -GI upset -Hypersensitivity -Photosensitivity -Hypoglycemia -C-diff |
Critical Thinking Activity 3.10a
Utilizing the above grid information, consider the following clinical scenario question:
A nurse is administering levofloxacin to a patient diagnosed with pneumonia. The patient reports that he has pain "above his heel" today. The nurse assesses and discovers the pain is over the Achilles tendon. What is the nurse's next best response?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
Aminoglycosides are a potent broad spectrum of antibiotics that are useful for treating severe infections. Many aminoglycosides are poorly absorbed in the GI tract; therefore, the majority are given IV or IM. Aminoglycosides are potentially nephrotoxic and neurotoxic. They should be administered cautiously. Blood peak and trough levels should be performed to titrate a safe dose for each patient.
Indications: Streptomycin is used for streptococcal endocarditis and a second line treatment for tuberculosis. Neomycin is used in the treatment of hepatic encephalopathy as adjunct therapy to lower ammonia levels and is also used as a bowel prep for colon procedures.
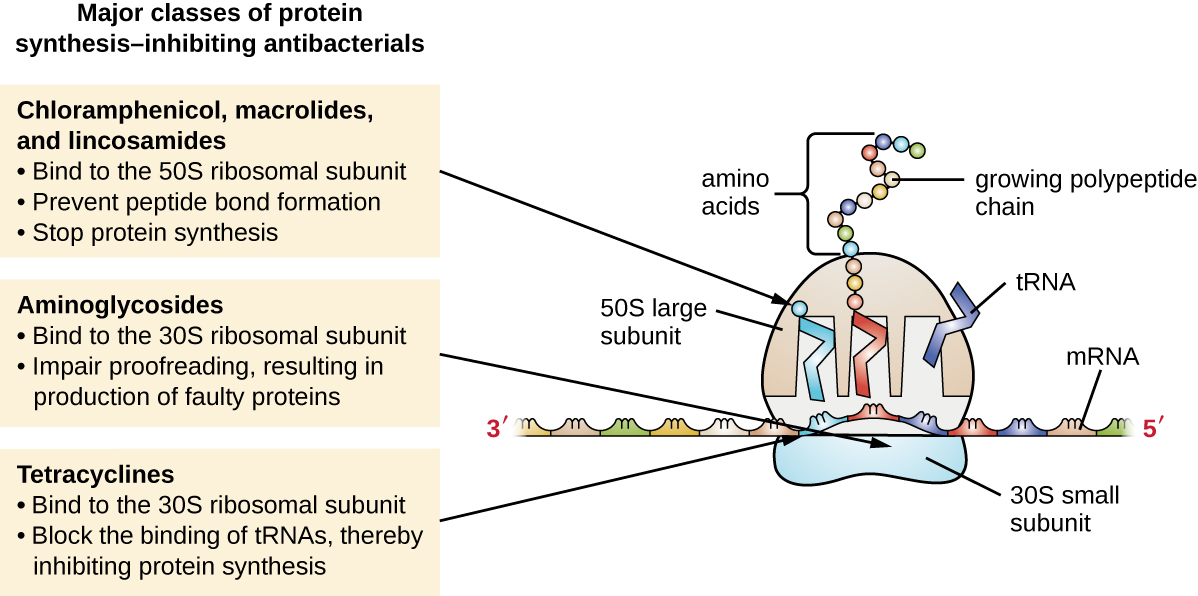
Mechanism of Action: Aminoglycosides are bactericidal and bind with the area of the ribosome known as the 30S subunit, inhibiting protein synthesis in the cell wall and resulting in bacterial death (see Figure 3.9).[4] Aminoglycosides may be given with beta-lactam medications to facilitate transport of aminoglycoside across the cellular membrane, resulting in a synergistic effect and increasing drug effectiveness.
Special Administration Considerations: Aminoglycosides can result in many adverse effects for the patient and, therefore, the nurse should monitor the patient carefully for signs of emerging concerns. Peak and trough levels are used to titrate this medication to a safe dose. Aminoglycosides can be nephrotoxic (damaging to kidney), neurotoxic (damaging to the nervous system), and ototoxic (damaging to the ear). Nurses should monitor the patient receiving aminoglycosides for signs of decreased renal function such as declining urine output and increasing blood urea nitrogen (BUN), creatinine, and declining glomerular filtration rate (GFR). Indications of damage to the neurological system may be assessed as increasing peripheral numbness or tingling in the extremities. Additionally, the patient should be carefully assessed for hearing loss or hearing changes throughout the course of drug administration.
Patient Teaching & Education: Patients receiving aminoglycosides should be advised to monitor for signs of hypersensitivity and auditory changes. This may include tinnitus and hearing loss. Patients may also experience accompanying vertigo while on the medication. Patients should be advised to drink plenty of fluids while taking the medication. Female patients should notify their provider if pregnancy is planned or if they are actively breastfeeding.[5]
Now let's take a closer look at the medication grid for streptomycin and gentamycin in Table 3.12.[6]
Table 3.12 Streptomycin and Gentamycin Medication Grid
Class/Subclass |
Prototype/Generic |
Administration Considerations |
Therapeutic Effects |
Side/Adverse Effects |
|---|---|---|---|---|
| Aminoglycosides | streptomycin | Check for allergies
Obtain culture before administering IM: Blood sample for peak level should be obtained 1 to 2 hours after IM injection; obtain blood for trough level just before next dose Inject in a large muscle Handle carefully; use gloves to prepare Monitor peak and trough levels |
Monitor for systemic signs of infection:
- WBCs - Fever Monitor actual site of infection Monitor culture results |
GI upset
Rash Report diarrhea immediately SAFETY: Nephrotoxicity: monitor renal function closely Risk for severe neurotoxic reactions, especially with renal impairment. Can result in respiratory paralysis if given soon after anesthesia or muscle relaxant Risk for ototoxicity, especially if administered with a loop diuretic Can cause harm to fetus and breastfed infants |
Critical Thinking Activity 3.12a
Using the above grid information, consider the following clinical scenario question:
A patient is admitted with streptococcal endocarditis and the nurse is preparing the morning dose of streptomycin. The lab has not yet arrived to obtain the trough level, and the drug is now overdue to be given. What is the nurse's next best response?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
Now that we have reviewed antimicrobial basics, administration considerations, and the nursing process when administering antimicrobials, we will take a closer look at specific antimicrobial classes and administration considerations, therapeutic effects, adverse effects, and specific teaching needed for each class of antimicrobials. Each of the following sections of this chapter is based on a class or subclass of anti-infective medications. Each section discusses the mechanism of action, specific administration considerations, and common patient teaching for this class/subclass of medication. Each section is then followed by a medication table with a common generic medication and its specific administration considerations, therapeutic effects, and side effects/adverse effects for this medication.
Penicillins
Penicillin was the first antibiotic discovered and its detection came as a bit of an accident. In 1928, Alexander Fleming, a professor of bacteriology at St. Mary's Hospital in London, discovered penicillin accidentally growing in a petri dish in his lab. The penicillin was the result of mold juice that had grown there inadvertently. Fleming noted that this "mold juice" inhibited the growth of Staphylococcus bacteria that was previously growing in the petri dish. Subsequently, the first antibiotic discovery was made.[7]
Indications: Penicillins are prescribed to treat a variety of infectious processes such as Streptococcal infections, Pneumococcal infections, and Staphylococcal infections. Penicillins may be administered orally, IV, or intramuscularly.
Mechanism of Action: Penicillins are bactericidal and kill bacteria by interfering with the synthesis of proteins needed in their cellular walls.[8] When the bacterial cell wall is impaired, the cell is rapidly broken down and destroyed.
Specific Administration Considerations: In addition to general antimicrobial administration considerations, it is important to monitor patients who receive penicillins for signs of superinfections such as C-diff or yeast infections. There is also a cross-sensitivity for patients allergic to cephalosporins. It is important to remember that patients who are prescribed high doses of penicillin may experience significant coagulation abnormalities.[9] Other notable drug interactions include the use of diuretic therapy with penicillin. Penicillin contains a significant amount of potassium. Patients receiving potassium-sparing diuretics or supplementation should be monitored for signs of hyperkalemia. Penicillin is best absorbed on an empty stomach; however, many patients may experience GI upset and subsequently take the medication with food.
Patient Teaching & Education: The patient should notify the health care provider (HCP) if fever or diarrhea develops, especially if the stool contains blood, pus, or mucus. Advise the patient not to treat diarrhea without advice from HCP. If GI upset occurs, the patient may take the medication with meals but should avoid taking with citrus-based products, which can impede absorption. Additionally, patients should be instructed to chew oral chewable tablets thoroughly before swallowing. The patient should report a rash or any signs of superinfection (black, furry overgrowth on tongue; vaginal itching or discharge; loose or foul-smelling stool).
Patients should be instructed to take medication around the clock and to finish the drug completely as directed. Doses should be spaced evenly to achieve the desired therapeutic effect. Additionally, patients should receive instruction to not share medication and that any sharing of medications may be dangerous. Patients with a history of rheumatic heart disease or valve replacement should receive instruction regarding the importance of using antimicrobial prophylaxis before invasive medical or dental procedures. Female patients taking oral contraceptives should use an alternative form of contraception during therapy with amoxicillin and until next period. Patients should notify their HCP if symptoms do not improve.[10]
Now let's take a closer look at the penicillin medication grid in Table 3.5.[11] Medication grids are intended to assist students to learn key points about each medication. Basic information related to a common generic medication in this class is outlined, including administration considerations, therapeutic effects, and side effects/adverse effects. Prototype/generic medications listed in the medication grid are also hyperlinked directly to a free resource from the United States National Library of Medicine called Daily Med. Because information about medication is constantly changing, nurses should always consult evidence-based resources to review current recommendations before administering specific medication. On the home page of Daily Med, enter the drug name in the search bar to read more about the medication.
Table 3.5 Penicillin Medication Grid
Class/Subclass |
Prototype-Generic |
Administration Considerations |
Therapeutic Effects |
Side/Adverse Effects |
|---|---|---|---|---|
| Penicillin | penicillin V (PO)
penicillin G (IV) piperacillin/tazobactam (combination product) |
Check for allergies to penicillin or cephalosporins
Obtain culture, if ordered, before first dose Take w/ full glass of water; no acidic juice Best absorbed orally on empty stomach; give with food if stomach upset If high doses; monitor INR, platelets, PT |
Monitor for systemic signs of infection:
-WBCs -Temp -Culture results Monitor actual site of infection for improvement |
Common: nausea, vomiting, epigastric distress, diarrhea, and black hairy tongue
Monitor for C-diff, candidiasis, and hyperkalemia Hypersensitivity: Rash (maculopapular to exfoliative dermatitis), urticaria, laryngeal edema, and anaphylaxis SAFETY: If an allergic reaction occurs, penicillin should be discontinued and appropriate therapy instituted. Serious anaphylactic reactions require emergency treatment with epinephrine and airway management |
Critical Thinking Activity 3.5a
Using the above grid information, consider the following clinical scenario question:
Mr. Jones was admitted to the medical surgical floor with a Pneumococcal respiratory infection and prescribed penicillin V 500 mg PO every 6 hours. You bring the patient his 0800 medications, which include his penicillin. The patient has just finished his breakfast that included orange juice. Would you proceed with the penicillin administration at this time? Why or why not?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
Now that we have reviewed antimicrobial basics, administration considerations, and the nursing process when administering antimicrobials, we will take a closer look at specific antimicrobial classes and administration considerations, therapeutic effects, adverse effects, and specific teaching needed for each class of antimicrobials. Each of the following sections of this chapter is based on a class or subclass of anti-infective medications. Each section discusses the mechanism of action, specific administration considerations, and common patient teaching for this class/subclass of medication. Each section is then followed by a medication table with a common generic medication and its specific administration considerations, therapeutic effects, and side effects/adverse effects for this medication.
Penicillins
Penicillin was the first antibiotic discovered and its detection came as a bit of an accident. In 1928, Alexander Fleming, a professor of bacteriology at St. Mary's Hospital in London, discovered penicillin accidentally growing in a petri dish in his lab. The penicillin was the result of mold juice that had grown there inadvertently. Fleming noted that this "mold juice" inhibited the growth of Staphylococcus bacteria that was previously growing in the petri dish. Subsequently, the first antibiotic discovery was made.[12]
Indications: Penicillins are prescribed to treat a variety of infectious processes such as Streptococcal infections, Pneumococcal infections, and Staphylococcal infections. Penicillins may be administered orally, IV, or intramuscularly.
Mechanism of Action: Penicillins are bactericidal and kill bacteria by interfering with the synthesis of proteins needed in their cellular walls.[13] When the bacterial cell wall is impaired, the cell is rapidly broken down and destroyed.
Specific Administration Considerations: In addition to general antimicrobial administration considerations, it is important to monitor patients who receive penicillins for signs of superinfections such as C-diff or yeast infections. There is also a cross-sensitivity for patients allergic to cephalosporins. It is important to remember that patients who are prescribed high doses of penicillin may experience significant coagulation abnormalities.[14] Other notable drug interactions include the use of diuretic therapy with penicillin. Penicillin contains a significant amount of potassium. Patients receiving potassium-sparing diuretics or supplementation should be monitored for signs of hyperkalemia. Penicillin is best absorbed on an empty stomach; however, many patients may experience GI upset and subsequently take the medication with food.
Patient Teaching & Education: The patient should notify the health care provider (HCP) if fever or diarrhea develops, especially if the stool contains blood, pus, or mucus. Advise the patient not to treat diarrhea without advice from HCP. If GI upset occurs, the patient may take the medication with meals but should avoid taking with citrus-based products, which can impede absorption. Additionally, patients should be instructed to chew oral chewable tablets thoroughly before swallowing. The patient should report a rash or any signs of superinfection (black, furry overgrowth on tongue; vaginal itching or discharge; loose or foul-smelling stool).
Patients should be instructed to take medication around the clock and to finish the drug completely as directed. Doses should be spaced evenly to achieve the desired therapeutic effect. Additionally, patients should receive instruction to not share medication and that any sharing of medications may be dangerous. Patients with a history of rheumatic heart disease or valve replacement should receive instruction regarding the importance of using antimicrobial prophylaxis before invasive medical or dental procedures. Female patients taking oral contraceptives should use an alternative form of contraception during therapy with amoxicillin and until next period. Patients should notify their HCP if symptoms do not improve.[15]
Now let's take a closer look at the penicillin medication grid in Table 3.5.[16] Medication grids are intended to assist students to learn key points about each medication. Basic information related to a common generic medication in this class is outlined, including administration considerations, therapeutic effects, and side effects/adverse effects. Prototype/generic medications listed in the medication grid are also hyperlinked directly to a free resource from the United States National Library of Medicine called Daily Med. Because information about medication is constantly changing, nurses should always consult evidence-based resources to review current recommendations before administering specific medication. On the home page of Daily Med, enter the drug name in the search bar to read more about the medication.
Table 3.5 Penicillin Medication Grid
Class/Subclass |
Prototype-Generic |
Administration Considerations |
Therapeutic Effects |
Side/Adverse Effects |
|---|---|---|---|---|
| Penicillin | penicillin V (PO)
penicillin G (IV) piperacillin/tazobactam (combination product) |
Check for allergies to penicillin or cephalosporins
Obtain culture, if ordered, before first dose Take w/ full glass of water; no acidic juice Best absorbed orally on empty stomach; give with food if stomach upset If high doses; monitor INR, platelets, PT |
Monitor for systemic signs of infection:
-WBCs -Temp -Culture results Monitor actual site of infection for improvement |
Common: nausea, vomiting, epigastric distress, diarrhea, and black hairy tongue
Monitor for C-diff, candidiasis, and hyperkalemia Hypersensitivity: Rash (maculopapular to exfoliative dermatitis), urticaria, laryngeal edema, and anaphylaxis SAFETY: If an allergic reaction occurs, penicillin should be discontinued and appropriate therapy instituted. Serious anaphylactic reactions require emergency treatment with epinephrine and airway management |
Critical Thinking Activity 3.5a
Using the above grid information, consider the following clinical scenario question:
Mr. Jones was admitted to the medical surgical floor with a Pneumococcal respiratory infection and prescribed penicillin V 500 mg PO every 6 hours. You bring the patient his 0800 medications, which include his penicillin. The patient has just finished his breakfast that included orange juice. Would you proceed with the penicillin administration at this time? Why or why not?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
