3.2 Antimicrobial Basics
Basic Concepts Related to Antimicrobial Therapy
Before we learn about medications that are used to treat infections in our patients, we must first understand the basics of microbiology. Let’s begin with a review of bacteria. Bacteria are found in nearly every habitat on earth, including within and on humans. Most bacteria are harmless or considered helpful, but some are pathogens. A pathogen is defined as an organism causing disease to its host. Pathogens, when overgrown, can cause significant health problems or even death for your patients.
Bacteria may be identified when a patient has an infection by using a culture and sensitivity test or a gram stain test. Antimicrobials may be classified as broad-spectrum or narrow-spectrum, based on the variety of bacteria they effectively treat. Additionally, antibiotics may be bacteriostatic or bactericidal in terms of how it targets the bacteria. Finally, the mechanism of action is also considered in the selection of an antibiotic.
In addition to antibiotics, antimicrobials also include medications used to treat viruses and fungi. Each of these topics will be discussed in more detail below, along with the issue of drug resistance.
Culture and Sensitivity
When a patient presents signs or symptoms of an infection, healthcare providers will begin the detective work needed to identify the source of the infection. A culture is a test performed to examine different body substances for the presence of bacteria or fungus.[1] These culture samples are commonly collected from a patient’s blood, urine, sputum, wound bed, etc. Nurses are commonly responsible for the collection of culture samples and must be conscientious to collect the sample prior to the administration of antibiotics. Antibiotic administration prior to a culture can result in a delayed identification of the organism and complicate the patient’s recovery. Once culture samples are collected, they are then incubated in a solution that promotes bacterial or fungal growth and spread onto a special culture plate.[2] Clinical microbiologists subsequently monitor the culture for signs of organism growth to aid in the diagnosis of the infectious pathogen. A sensitivity analysis is often performed to select an effective antibiotic to treat the microorganism. If the organism shows resistance to the antibiotics used in the test, those antibiotics will not provide effective treatment for the patient’s infection. Sometimes a patient may begin antibiotic treatment for an infection, but will be switched to a different, more effective antibiotic based on the culture and sensitivity results.[3]
Gram Positive vs. Gram Negative
A gram stain is another type of test that is used to assist in classification of pathogens. Gram stains are useful for quickly identifying if bacteria are “gram positive” or “gram negative,” based on the staining patterns of their cellular walls. Utilizing gram stain allows microbiologists to look for characteristic violet (Gram +) or red/pink (Gram -) staining patterns when they examine the organisms under a microscope.[4] Identification of bacteria as gram positive or gram negative assists the healthcare provider in quickly selecting an appropriate antibiotic to treat the infection.
Sample Gram Positive Infections
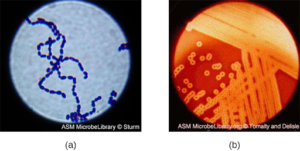
Streptococcus, the name which comes from the Greek word for twisted chain, is responsible for many types of infectious diseases in humans. Streptococcus is an example of a Gram + infection and is identified by its ability to lyse, or breakdown, red blood cells when grown on blood agar.
S. pyogenes is a type of β-hemolytic Streptococcus. This species is considered a pyogenic pathogen because of the associated pus production observed with infections it causes (see Figure 3.1[5] for an image of Streptococcus undergoing gram staining). S. pyogenes is the most common cause of bacterial pharyngitis (strep throat); it is also a common cause of various skin infections that can be relatively mild (e.g., impetigo) or life threatening (e.g., necrotizing fasciitis, also known as flesh-eating disease).[6]

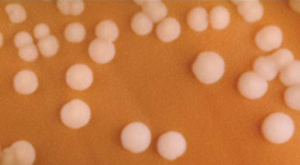
Staphylococcus is a second example of a Gram + bacteria. The bacteria Staphylococcus comes from a Greek word for bunches of grapes, which describes their microscopic appearance in culture. Strains of S. aureus cause a wide variety of infections in humans, including skin infections that produce boils, carbuncles, cellulitis, or impetigo. Many strains of S. aureus have developed resistance to antibiotics. Some antibiotic-resistant strains are designated as methicillin-resistant S. aureus (MRSA) and vancomycin-resistant S. aureus (VRSA) . These strains are some of the most difficult to treat because they exhibit resistance to nearly all available antibiotics, not just methicillin and vancomycin. Because they are difficult to treat with antibiotics, infections can be lethal. MRSA and VRSA are also contagious, posing a serious threat in hospitals, nursing homes, dialysis facilities, and other places where there are large populations of elderly, bedridden, and/or immunocompromised patients.[7] See Figure 3.2[8] for an image of Staphylococcus bacteria microscopically.
Sample Gram Negative Infections
Gram negative bacteria often grow between aerobic and anaerobic areas (such as in the intestines). Some gram negative bacteria cause severe, sometimes life-threatening disease. The genus Neisseria, for example, includes the bacteria N. gonorrhoeae, the causative agent of the sexually transmitted infection gonorrhea, and N. meningitides, the causative agent of bacterial meningitis. See Figure 3.3[9] for an image of Neisseria meningitides. Another common gram negative infection that is seen in hospitalized patients is Escherichia coli (E. Coli). This is a frequent culprit for urinary tract infections due to its presence in the GI tract.
Broad-Spectrum vs. Narrow-Spectrum Antimicrobials
Spectrum of activity is one of the factors that providers use when selecting antibiotics to treat a patient’s infection. A narrow-spectrum antimicrobial targets only specific subsets of bacterial pathogens.[10] For example, some narrow-spectrum drugs only target gram positive bacteria, but others target only gram negative bacteria. If the pathogen causing infection has been identified in a culture and sensitivity test, it is best to use a narrow-spectrum antimicrobial and minimize collateral damage to the normal microbacteria.
A broad-spectrum antimicrobial targets a wide variety of bacterial pathogens, including both gram positive and gram negative species, and is frequently used to cover a wide range of potential pathogens while waiting on the laboratory identification of the infecting pathogen. Broad-spectrum antimicrobials are also used for polymicrobial infections (a mixed infection with multiple bacterial species) or as prophylactic prevention of infections with surgery/invasive procedures. Finally, broad-spectrum antimicrobials may be selected to treat an infection when a narrow-spectrum drug fails because of development of drug resistance by the target pathogen.[11]
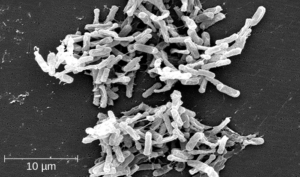
One risk associated with using broad-spectrum antimicrobials is that they will also target a broad spectrum of the normal microbacteria that can cause diarrhea. They also increase the risk of a superinfection , a secondary infection in a patient having a preexisting infection. A superinfection develops when the antibacterial intended for the preexisting infection kills the protective microbiota, allowing another pathogen resistant to the antibacterial to proliferate and cause a secondary infection. Common examples of superinfections that develop as a result of antimicrobial use include yeast infections (candidiasis) and pseudomembranous colitis caused by Clostridium difficile (C-diff), which can be fatal.[12] Probiotics, such as lactobacillus, are commonly used for individuals with C-diff to introduce normal bacteria into the gastrointestinal system and improve bowel function. See Figure 3.4[13] for an image of C-diff microscopically.
Let’s recap…
- A broad-spectrum antibiotic will treat gram positive and gram negative bacteria.
- A narrow-spectrum antibiotic will treat either gram positive or gram negative bacteria.
If a patient is started on an antibiotic that is gram + and the culture identifies a gram – organism, the medication will not improve the patient’s status. The selection of an incorrect antibiotic can lead to adverse reactions and increase bacterial resistance.
At times, a broad spectrum antibiotic may be administered prior to receiving the culture report due to the severity of the illness of the patient. Once the culture is reported, the antibiotic therapy is tailored to the patient. It is the nurse’s responsibility to review culture results and ensure that the results have been communicated to the prescribing provider.
Antibacterials Actions — Bacteriostatic vs. Bactericidal
When a provider selects an antibacterial drug, it is important to consider how and where the drug will ultimately target the bacteria. Antibacterial drugs can be either bacteriostatic or bactericidal in their interactions with the offending bacteria. Bacteriostatic drugs cause bacteria to stop reproducing; however, they may not ultimately kill the bacteria. In contrast, bactericidal drugs kill their target bacteria.
The decision about whether to use a bacteriostatic or bactericidal drug often depends on the type of infection and the overall immune status of the patient. In a healthy patient with strong immune defenses, both bacteriostatic and bactericidal drugs can be effective in achieving clinical cure. However, when a patient is immunocompromised, a bactericidal drug is essential for the successful treatment of infections. Regardless of the immune status of the patient, life-threatening infections such as acute endocarditis require the use of a bactericidal drug to eliminate all offending bacteria.[14]
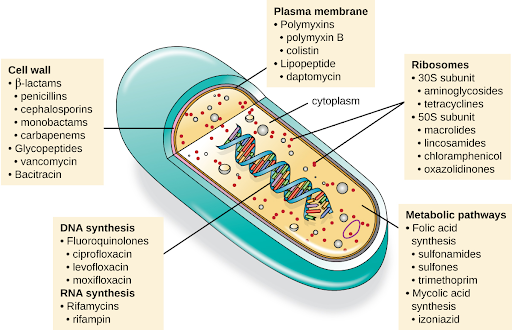
Mechanism of Action
Another consideration in the selection of an antibacterial drug is the drug’s mechanism of action. Each class of antibacterial drugs has a unique mechanism of action , the way in which a drug affects microbes at the cellular level. For example, cephalosporins act on the integrity of the cell wall. In contrast, aminoglycosides impact ribosome function and inhibit protein synthesis, which stops the proliferation of cells.[15] See Figure 3.5[16] for a summary of how various antibiotics affect the cell wall, the plasma membrane, the ribosomes, the metabolic pathways, or DNA synthesis of bacteria.
Antiviral
Similar to antibacterial medications, antiviral drugs directly impact interaction and reproduction of the offending microorganism. Antibacterial medications are required for treating bacterial infections; antivirals treat specific viral infections. For example, oseltamivir (Tamiflu) is commonly prescribed to treat influenza. Unlike antimicrobials, antiviral medications do not kill the offending virus, but they work to reduce replication and development of the virus.[17]
Antifungal
Antifungal, or antimycotic agents, are medications that are used to treat fungal infections. These medications work by killing the cells of the fungus or inhibiting the reproduction of the cells. Unlike antibacterial and antiviral medications, many antifungals are applied topically to the affected area. Fungal infections commonly affect surface areas of the body, including the toes, nails, mouth, groin, etc. For example, Candida albicans is a type of fungi that when overgrown in the mouth produces oral thrush. Patients experiencing thrush may be prescribed oral antifungal swish and spit medication such as nystatin.
Drug Resistance
Although there is a wide availability of medications that are useful for treating infection, greater limitations in effectiveness are being seen. According to the Centers for Disease Control (2019), each year in the United States, at least 2 million people are infected with an antibiotic-resistant infection, and more than 23,000 die.[18]
Prevention Strategies
In the United States and many other countries, most antimicrobial drugs are self-administered by patients at home. Unfortunately, many patients stop taking antimicrobials once their symptoms dissipate and they feel better. If a 10-day course of treatment is prescribed, many patients only take the drug for 5 or 6 days, unaware of the negative consequences of not completing the full course of treatment.
The Problem: A shorter course of treatment not only fails to kill the target organisms to the expected levels but also assists in creating drug-resistant variants within the body. A patient’s nonadherence amplifies drug resistance when the recommended course of treatment is long.
For example, treatment for tuberculosis (TB) has a recommended treatment regimen lasting from 6 months to a year. The CDC estimates that about one third of the world’s population is infected with TB, most living in underdeveloped or underserved regions where antimicrobial drugs are available over the counter. In such countries, there may be even lower rates of adherence than in developed areas. Nonadherence leads to antibiotic resistance and more difficulty in controlling pathogens. As a direct result, the emergence of multidrug-resistant strains of TB is becoming a huge problem.
The over prescription of antimicrobials also contributes to antibiotic resistance. Patients often demand antibiotics for diseases that do not require them, like viral colds and ear infections. Pharmaceutical companies aggressively market drugs to physicians and clinics, making it easy for them to give free samples to patients, and some pharmacies even offer certain antibiotics free to low-income patients with a prescription.
In recent years, various initiatives have aimed to educate parents and clinicians about the judicious use of antibiotics. However, previous studies have shown the parental expectations for antimicrobial prescriptions for children actually increased.
One possible solution that is being explored is a regimen called directly observed therapy (DOT), which involves the supervised administration of medications to patients. Patients are either required to visit a health-care facility to receive their medications, or health-care professionals must administer medication in patients’ homes or another designated location. DOT has been implemented in many cases for the treatment of TB and has been shown to be effective; indeed, DOT is an integral part of WHO’s global strategy for eradicating TB.
But is this a practical strategy for all antibiotics? Would patients taking penicillin, for example, be more or less likely to adhere to the full course of treatment if they had to travel to a health-care facility to receive each dose? Who would pay for the increased cost associated with DOT? When it comes to overprescription, should providers or drug companies be policed when it comes to over prescribing antibiotics to enforce best practices? What group should assume this responsibility, and what penalties would be effective in discouraging overprescription?
This is a complex issue with no clear, easy solution. However, what is clear is that all patients need extensive education regarding the judicious and complete use of medications to increase adherence and decrease the opportunity for antimicrobial resistance.[19]
Critical Thinking Activity 3.2a
Reflecting on current healthcare challenges regarding the ongoing emergence of antimicrobial resistant organisms, what actions could you take within your nursing practice to help prevent drug resistance?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” sections at the end of the book.
Interactive Activity
- This work is a derivative of Microbiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction. ↵
- Kristof, K. and Pongracz, J. (2016). Interpretation of blood microbiology results - function of the clinical microbiologist. The Journal of the International Federation of Clinical Chemistry and Laboratory Medicine, 27(2), 147-155. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4975230/ ↵
- Vorvick, L. (Ed.). (2019, February 7). Sensitivity analysis. https://medlineplus.gov/ency/article/003741.htm ↵
- This work is a derivative of Microbiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- "OSC Microbio 04 04 Strep.jpg" by CNX OpenStax is licensed under CC BY 4.0 Access for free at https://openstax.org/books/microbiology/pages/4-4-gram-positive-bacteria ↵
- This work is a derivative of Microbiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of "CDC-10046-MRSA.jpg" by Janice Haney Carr, Centers for Disease Control and Prevention is licensed under CC0 ↵
- "OSC Microbio 04 02 Neisseria.jpg" by CNX OpenStax is licensed under CC BY 4.0 Access for free at https://openstax.org/books/microbiology/pages/4-2-proteobacteria ↵
- This work is a derivative of Microbiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction. ↵
- This work is a derivative of Microbiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of "Clostridium difficile 01.jpg" by Lois D Wiggs at Centers of Disease Control and Prevention is licensed under CC0 ↵
- This work is a derivative of Microbiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- "OSC Microbio 14 02 Modes.jpg" by CNX Openstax is licensed under CC BY 4.0 Access for free at https://openstax.org/books/microbiology/pages/14-3-mechanisms-of-antibacterial-drugs ↵
- This work is a derivative of Microbiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- Centers for Disease Control and Prevention. (2019). About antimicrobial resistance. https://www.cdc.gov/drugresistance/about.html ↵
- This work is a derivative of Microbiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
Pancreatic Basics: A&P Review
Pancreas
The pancreas is a long, slender organ located near the stomach (see Figure 9.7).[1] Although it is primarily an exocrine gland, secreting a variety of digestive enzymes, the pancreas also has an endocrine function. Pancreatic islets, clusters of cells formerly known as the islets of Langerhans, secrete glucagon and insulin. Glucagon plays an important role in blood glucose regulation because low blood glucose levels stimulate its release. On the other hand, elevated blood glucose levels stimulate the release of insulin.

Regulation of Blood Glucose Levels by Insulin and Glucagon
Glucose is the preferred fuel for all body cells. The body derives glucose from the breakdown of the carbohydrate-containing foods and drinks we consume. Glucose not immediately taken up by cells for fuel can be stored by the liver and muscles as glycogen or converted to triglycerides and stored in the adipose tissue. Hormones regulate both the storage and the utilization of glucose as required. Receptors located in the pancreas sense blood glucose levels, and subsequently, the pancreatic cells secrete glucagon or insulin to maintain normal levels.
Glucagon
Receptors in the pancreas can sense the decline in blood glucose levels, such as during periods of fasting or during prolonged labor or exercise. In response, the alpha cells of the pancreas secrete the hormone glucagon, which has several effects:
- It stimulates the liver to convert stores of glycogen back into glucose. This response is known as glycogenolysis. The glucose is then released into the circulation for use by body cells.
- It stimulates the liver to take up amino acids from the blood and convert them into glucose. This response is known as gluconeogenesis.
- It stimulates lipolysis, the breakdown of stored triglycerides into free fatty acids and glycerol. Some of the free glycerol released into the bloodstream travels to the liver, which converts it into glucose. This is also a form of gluconeogenesis.
Taken together, these actions increase blood glucose levels. The activity of glucagon is regulated through a negative feedback mechanism; rising blood glucose levels inhibit further glucagon production and secretion. (See Figure 9.8 for an illustration of homeostatic regulation of blood glucose levels.)[2]
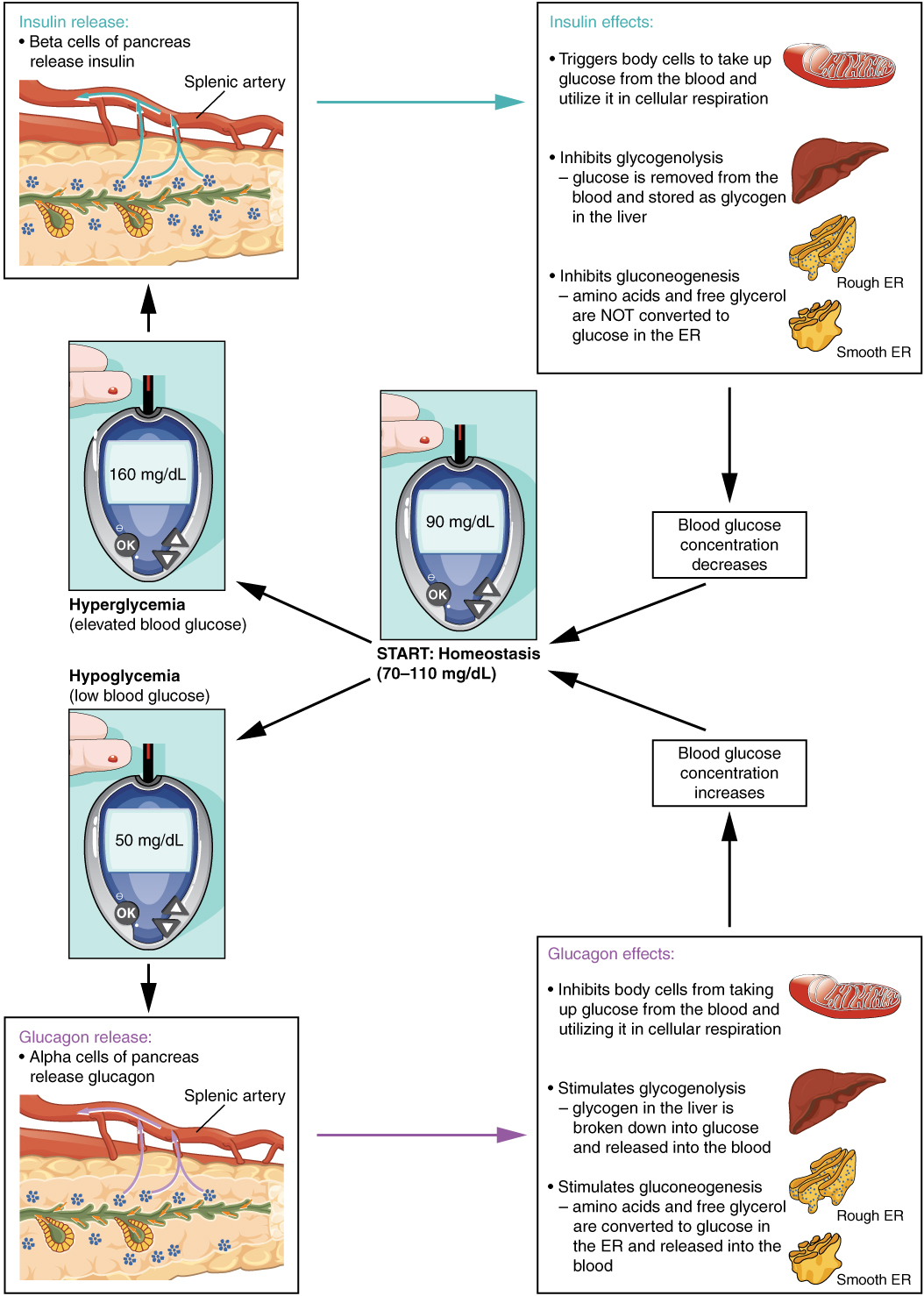
Insulin
Insulin facilitates the uptake of glucose into skeletal and adipose body cells. The presence of food in the intestine triggers the release of gastrointestinal tract hormones. This, in turn, triggers insulin production and secretion by the beta cells of the pancreas. Once nutrient absorption occurs, the resulting surge in blood glucose levels further stimulates insulin secretion.
Insulin triggers the rapid movement of glucose transporter vesicles to the cell membrane, where they are exposed to the extracellular fluid. The transporters then move glucose by facilitated diffusion into the cell interior.
Insulin also reduces blood glucose levels by stimulating glycolysis, the metabolism of glucose for generation of ATP. It further stimulates the liver to convert excess glucose into glycogen for storage, and it inhibits enzymes involved in glycogenolysis and gluconeogenesis. Finally, insulin promotes triglyceride and protein synthesis. The secretion of insulin is regulated through a negative feedback mechanism. As blood glucose levels decrease, further insulin release is inhibited.
Disorders of the Endocrine System: Diabetes Mellitus
Dysfunction of insulin production and secretion, as well as the target cells’ responsiveness to insulin, can lead to a condition called diabetes mellitus, a common disease that affects the ability of the body to produce and/or utilize insulin. There are two main forms of diabetes mellitus. Type 1 diabetes is an autoimmune disease affecting the beta cells of the pancreas. The beta cells of people with type 1 diabetes do not produce insulin; thus, synthetic insulin must be administered by injection or infusion. Type 2 diabetes accounts for approximately 95 percent of all cases. It is acquired, and lifestyle factors such as poor diet and inactivity greatly increase a person’s risk. In type 2 diabetes, the body’s cells become resistant to the effects of insulin. In response, the pancreas increases its insulin secretion, but over time, the beta cells become exhausted. In many cases, type 2 diabetes can be reversed by moderate weight loss, regular physical activity, and consumption of a healthy diet. However, if blood glucose levels cannot be controlled, oral diabetic medication is implemented and eventually the type 2 diabetic may require insulin.
Diabetes is diagnosed when lab tests reveal that blood glucose levels are higher than normal, a condition called hyperglycemia.[3] According to the American Diabetes Association (ADA), normal fasting blood glucose levels are 80-130 mg/dL. Glycosylated hemoglobin, also called A1C, is used to assess long-term blood glucose levels over 3 months. The ADA states that A1C target levels vary according to age and health, but the generalized A1C target is less than 7%.[4]
Nursing Considerations
Assessment
Diabetic patients should be continuously monitored for signs of hypoglycemia and hyperglycemia. When a diabetic patient is experiencing stress or an infection, the nurse should plan to assess the blood glucose levels more frequently.
Implementation
The nurse should follow agency policy and ISMP guidelines for safe insulin administration. See the "Legal Ethical" chapter for more information about ISMP guidelines. Onset and peak times of insulin and sulfonylureas, in association with anticipated meal times, should always be considered to avoid hypoglycemia episodes. If a hypoglycemia episode occurs, the nurse should intervene quickly using the agency’s established hypoglycemia protocol, and the event should be reported to the provider and in the shift-to-shift report. Symptomatic hyperglycemia should be immediately reported to the provider. Patient education should be provided to patients, family members, and/or caregivers according to ADA and ISMP guidelines.
Evaluation
The nurse should evaluate A1C levels to determine effectiveness (and compliance with) the treatment regimen.
Diabetic Medication Classes: Insulins
Because the hallmark of type 1 diabetes is absent or near-absent β-cell function, insulin treatment is essential for individuals with type 1 diabetes. Current evidence-based recommendations regarding pharmacological treatment of type 1 diabetes from the American Diabetes Association (ADA) include:
- Most people with type 1 diabetes should be treated with multiple daily injections of prandial and basal insulin or continuous subcutaneous insulin infusion.
- Most individuals with type 1 diabetes should use rapid-acting insulin analogs to reduce hypoglycemia risk.
- Individuals with type 1 diabetes on prandial insulin doses should be educated on carbohydrate intake, premeal blood glucose levels, and anticipated physical activity.
- Individuals with type 1 diabetes who have been successfully using continuous subcutaneous insulin infusion should have continued access to this therapy after they turn 65 years of age.
Basal insulin can be long-acting (insulin glargine or insulin detemir) or intermediate-acting (insulin isophane suspension [NPH]). Prandial insulins are used with meals and may be rapid acting (insulin lispro, insulin aspart, or insulin glulisine) or short acting (regular insulin).
According to the ADA, insulin requirements can be estimated based on weight, with typical doses ranging from 0.4 to 1.0 units/kg/day. Higher amounts are required during puberty, pregnancy, and medical illness. Physiologic insulin secretion varies with glycemia, meal size, and tissue demands for glucose. To approach this variability in people using insulin treatment, strategies have evolved to adjust meal-time doses based on predicted needs. Thus, education of patients on how to adjust insulin to account for carbohydrate intake, premeal glucose levels, and anticipated activity is important. Ensuring that patients and/or caregivers understand correct insulin injection technique is also important to optimize glucose control and insulin use safety.[5]
Patients on insulin therapy are at risk for hypoglycemia. It is essential for the nurse to monitor for signs of hypoglycemia and to intervene appropriately. See Figure 9.9 for symptoms of hypoglycemia. Hypoglycemia is defined as a blood glucose level below 70 mg/dL; severe hypoglycemia refers to a blood glucose level below 40 mg/dL.
Hypoglycemia Symptoms
| Mild-to-Moderate | Severe |
|---|---|
|
|
Figure 9.9 Hypoglycemia Symptoms
If a patient with diabetes shows a sudden change in mood or mental status or other symptoms of hypoglycemia, the nurse should immediately check the blood glucose level. Healthcare agencies use hypoglycemia protocols so that the nurse can react quickly to episodes of hypoglycemia before they become severe. Hypoglycemia protocols contain orders for immediate treatment by the nurse. For instance, in patients who can tolerate oral intake, 15 grams of rapidly digested carbohydrates (such as 4 ounces of fruit juice) are recommended. In patients who are NPO or can’t take oral treatment, dextrose 50% IV or glucagon IM or subcutaneously are administered. Patients who have had a hypoglycemic episode should be monitored closely for the following 24 hours because they are at increased risk for another episode. The provider and the oncoming nurse should be notified of hypoglycemia episodes to discuss the possible cause of the hypoglycemic event and make insulin adjustments, if needed, to avoid additional hypoglycemia. Tracking hypoglycemia episodes and analyzing causes are important performance improvement activities.[6]
The arrival of continuous glucose monitors to clinical practice has been proven to reduce nocturnal hypoglycemia in people using insulin pumps with glucose sensors due to automatic suspension of insulin delivery at a preset glucose level. The U.S. Food and Drug Administration has also approved the first hybrid closed-loop pump system.[7] A hybrid closed-loop pump system automatically adjusts basal insulin delivery every 5 minutes based on sensor glucose to maintain blood glucose levels as close to a specific target as possible.[8]
According to the ADA, lifestyle modifications that improve health should be emphasized, along with any pharmacologic therapy. Lifestyle modifications include healthy food choices to stabilize blood glucose levels, as well as daily exercise.
Hypokalemia
All insulin products cause a shift in potassium from the extracellular to intracellular space, which can possibly lead to hypokalemia. Untreated hypokalemia may cause respiratory paralysis, ventricular arrhythmia, and death. Monitor potassium levels in patients at risk for hypokalemia due to other medications such as diuretics.
Insulin Pens
Insulin pens are often used in inpatient settings, as well as for self-administration, to facilitate safe and accurate self-administration of insulin. See Figure 9.10 for an image of an insulin pen.[9] According to the ISMP, insulin pens offer several advantages over vials beyond dosing accuracy, convenience, and ease of use:
- Each pen is already labeled by the manufacturer with the product name and product barcode (whereas syringes of insulin prepared on the patient care unit from vials run the risk of being unlabeled).
- Each pen can be individually labeled with the patient’s name (and ideally with a patient-specific barcode).
- The pen provides the patient’s insulin in a form ready for administration.
- The pen lessens nursing time needed to prepare and administer insulin.
- Insulin pens reduce medication waste that can occur when dispensing 10 mL-sized insulin vials for each patient.
However, improper sharing of insulin pens among multiple patients has exposed patients to bloodborne pathogens. Insulin pens should never be reused for multiple patients; even if the needle is changed between patients, there can still be body fluid exposure.[10]

High-Alert Medication and Prevention of Errors
Insulin is a high-alert medication that can be associated with significant patient harm when used in error. A variety of error types have been associated with insulin therapy, including administration of the wrong insulin product, improper dosing (underdosing and overdosing), dose omissions, incorrect use of insulin delivery devices, wrong route (intramuscular versus subcutaneous), and improper patient monitoring. Many errors result in serious hypoglycemia or hyperglycemia. Hypoglycemia is often caused by a failure to adjust insulin therapy in response to a reduction in nutritional intake or an excessive insulin dose stemming from a prescribing or dose measurement error. Other factors that contribute to serious hypoglycemia include inappropriate timing of insulin doses with food intake, creatinine clearance, body weight, changes in medications that affect blood glucose levels, poor communication during patient transfer to different care teams, and poor coordination of blood glucose testing with insulin administration at meal time.
In an inpatient setting, manifestations of poor glycemic control, including severe hypoglycemia and hyperglycemia, are deemed hospital-acquired conditions by the Centers for Medicare and Medicaid Services (CMS). CMS notes that poor glycemic control can be reasonably prevented with implementation of evidence-based guidelines; thus, the CMS denies payment for diabetic ketoacidosis, hypoglycemic coma, and other serious conditions related to poor glycemic control. Agency policies and procedures should be closely followed to avoid these errors and manifestations of poor glycemic control.
One strategy for look-alike medications such as Humalog and Humalin is tall man lettering on the label. Tall man lettering describes a method for differentiating the unique letter characters of similar drug names known to be confused with one another, such as HumaLOG and HumaLIN.
ISMP recommends the following safe practice guidelines for the administration of insulin by the nurse:
- Patient-specific insulin pens are stored on clinical units in a manner that prevents their inadvertent use on more than one patient.
- A coordinated process is developed to ensure timely blood glucose checks and administration of prandial insulin in conjunction with meal delivery.
- Verbal communication of point-of-care blood glucose value results are avoided as much as possible and are NEVER routinely used as the only source of information when determining insulin doses.
- Appropriately label all clinician-prepared syringes of subcutaneous insulin, unless the medication is prepared at the patient’s bedside and is immediately administered to the patient without any break in the process.
- Prior to subcutaneous insulin administration, the practitioner:
- Confirms that there is an appropriate indication
- Assesses the patient’s most current blood glucose value
- Assesses the patient for symptoms of hypoglycemia
- Informs the patient of their most current blood glucose level
- Informs the patient of their dose, the full name of the product, and the insulin’s intended action
- An individual insulin pen is never used for more than one patient.
- Barcode scanning is used to verify that a patient-specific pen is used to administer the correct insulin to the correct patient.
- Prior to transitions of care, a process is in place to ensure that patients will have the necessary prescriptions, supplies, a follow-up care plan, and printed instructions for all prescribed insulin and blood glucose monitoring.
- Patients discharged on insulin are assessed for understanding of their self-management, including:
- Demonstration of proper dose measurement and self-administration using the same administration device that will be used at home (e.g., vial and syringe, pen, pump)
- Correct monitoring of blood glucose values
- The signs and symptoms of hyper- and hypoglycemia and how to respond if these symptoms occur
- Common types of errors possible with their insulin therapy and how to prevent or detect these errors
- The importance of regular follow-up with their primary care provider/specialist, including the date of their next appointment
- Patients who self-administer concentrated U-500 insulin using a vial and syringe are taught to use only a U-500 syringe and communicate their doses in terms of the name and concentration of the insulin and the actual dose in units using only the U-500 syringe[11]
Lifespan Considerations
Elderly
The elderly are at higher risk for hypoglycemia episodes. The ADA has the following recommendations for elderly patients with diabetes:
- In older adults at increased risk of hypoglycemia, medication classes with low risk of hypoglycemia are preferred.
- Overtreatment of diabetes is common in older adults and should be avoided.
- Deintensification (or simplification) of complex regimens is recommended to reduce the risk of hypoglycemia, if it can be achieved within the individualized A1C target.[12]
Children and Adolescents
Type 1 diabetes is the most common form of diabetes in youth. Unique aspects of care and management of children and adolescents with type 1 diabetes must be considered, such as changes in insulin sensitivity related to physical growth and sexual maturation, ability to provide self-care, supervision in the child care and school environment, neurological vulnerability to hypoglycemia and hyperglycemia in young children, as well as possible adverse neurocognitive effects of diabetic ketoacidosis (DKA). Evidence-based ADA recommendations for glycemic control for children and adolescents include:
- The majority of children and adolescents with type 1 diabetes should be treated with intensive insulin regimens, either via multiple daily injections or continuous subcutaneous insulin infusion.
- All children and adolescents with type 1 diabetes should self-monitor glucose levels multiple times daily (up to 6–10 times/day), including pre-meal, pre-bedtime, and as needed for safety in specific situations such as exercise, driving, or the presence of symptoms of hypoglycemia.
- Continuous glucose monitoring should be considered in all children and adolescents with type 1 diabetes, whether using injections or continuous subcutaneous insulin infusion, as an additional tool to help improve glucose control. Benefits of continuous glucose monitoring correlate with adherence to ongoing use of the device.
- Automated insulin delivery systems appear to improve glycemic control and reduce hypoglycemia in children and should be considered in children with type 1 diabetes.
- An A1C target of <7.5% should be considered in children and adolescents with type 1 diabetes but should be individualized based on the needs and situation of the patient and family. [13]
There are several different types of insulins that vary in terms of onset, peak, and duration. It is critical for the nurse to be knowledgeable of these differences to help prevent episodes of hypoglycemia due to mismatched administration of insulin with food intake.
Rapid-Acting Insulin
Rapid-acting insulins include insulin lispro (Humalog) and insulin aspart (Novolog) and are also available via inhalation (Afrezza). See Figure 9.11 for an image of Novolog insulin.[14]

Indications
Rapid-acting insulins are also called prandial insulins because they are administered with meals to mimic the effects of endogenous insulin release when food is eaten. Dosages of rapid-acting insulin are individualized based on carbohydrate intake, premeal glucose levels, and anticipated activity.
Mechanism of Action
Insulins lower blood glucose by stimulating peripheral glucose uptake by skeletal muscle and fat and by inhibiting hepatic glucose production.
Specific Administration Considerations
Humalog-100 (100 units per ml) and Humalog-200 (200 units per ml) are administered subcutaneously; however, only Humalog-100 is administered via continuous subcutaneous injection or intravenously. Humalog-100 can only be mixed with NPH insulin, but Humalog-200 should not be mixed with other insulin. Inspect insulin visually before use. It should appear clear and colorless; do not use if particulate matter or coloration is seen. Humalog-100 is available in vials, KwikPens, and cartridges; Humalog-200 is only available in KwikPens. Administer subcutaneously into the outer lateral aspect of the upper arm, the abdomen (from below the costal margin to the iliac crest and more than two inches from the umbilicus), the anterior upper thighs, or the buttocks. Rotate injection sites within the same region from one injection to the next to reduce the risk of lipodystrophy. Lipodystrophy can be a lump or small dent in the skin that forms when a person performs injections repeatedly in the same spot.
Because of the rapid onset of insulin lispro and insulin aspart and the potential for hypoglycemia, these insulins should be administered within 15 minutes before or right after eating a meal. Peak serum levels are seen 30 to 90 minutes after dosing. Inhaled insulin enters the bloodstream within 1 minute and peaks in 30-60 minutes. Inhaled insulin is contraindicated in patients with chronic lung disease such as asthma or COPD.
Adverse effects of all insulins include hypoglycemia and hypokalemia. Inhaled insulin has a Black Box Warning for potentially causing acute bronchoconstriction.
Patient Teaching & Education
See ISMP guidelines for patient teaching in the previous section titled “High Risk Medications and Prevention of Errors.”
Short-Acting Insulin
Short-acting insulins include regular insulin with a brand name of Humulin R or Novolin R. A concentrated formulation of Humulin R u-500 is also available. See Figure 9.12 for an image of Humulin R insulin.[15]

Indications
Short-acting insulins are given with meals to mimic the effects of endogenous insulin release when food is eaten. Dosages of short-acting insulin are individualized based on carbohydrate intake, premeal glucose levels, and anticipated activity levels.
Mechanism of Action
The primary activity of insulin is the regulation of glucose metabolism. Insulin lowers blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production.
Specific Administration Considerations
Regular insulin is generally administered subcutaneously. It is the only insulin that can be administered intravenously under close supervision of blood glucose and potassium levels. It is available in vials and insulin pens. Inspect insulin visually before use. It should appear clear and colorless; do not use if particulate matter or coloration is seen. Administer subcutaneously into the outer lateral aspect of the upper arm, the abdomen (from below the costal margin to the iliac crest and more than two inches from the umbilicus), the anterior upper thighs, or the buttocks. Rotate injection sites within the same region from one injection to the next to reduce the risk of lipodystrophy. Subcutaneous doses should be administered approximately 30 minutes before meals because this is the typical onset of action. Peak effects occur in 3 hours with a duration of 8 hours. Do not mix with insulin preparations other than NPH.
Humulin R u-500 should only be administered in u-500 insulin syringes to avoid dosage calculation errors.
Adverse effects of insulin include hypoglycemia and hypokalemia.
Patient Teaching & Education
See IMSP guidelines for patient teaching in the previous section entitled “High Risk Medications and Prevention of Errors.”
Intermediate-Acting Insulin
NPH insulin, also known as isophane insulin, is an intermediate–acting insulin. Brand names include Humulin-N or Novolin-N. Mixtures of short- and intermediate-acting insulin include Humulin 70/30 or Novolin 70/30.
Indications
Intermediate insulins are administered once or twice daily to mimic endogenous basal insulin levels.
Mechanism of Action
Insulins lower blood glucose by stimulating peripheral glucose uptake by skeletal muscle and fat and by inhibiting hepatic glucose production.
Specific Administration Considerations
NPH insulin is a white and cloudy suspension. Gently roll or invert vial/pen several times to re-suspend the insulin before administration. It should only be administered subcutaneously. It may be mixed with rapid-acting or short-acting insulins, but those insulins should be drawn into the syringe before the NPH is added. Administer subcutaneously into the outer lateral aspect of the upper arm, the abdomen (from below the costal margin to the iliac crest and more than two inches from the umbilicus), the anterior upper thighs, or the buttocks. Rotate injection sites within the same region from one injection to the next to reduce the risk of lipodystrophy. The onset of action and peak are affected by the site of injection, physical activity level, and other variables but the median peak level occurs in 4 hours. See Figure 9.13 for an image of Novolin-N (a cloudy insulin) that can be mixed with Novolin R (a clear insulin).[16]

Mixed medications such as Humulin 70/30 should be administered subcutaneously approximately 30 minutes before a meal. They are typically dosed twice daily (with each dose intended to cover 2 meals or a meal and a snack).
Unopened vials should be stored in the refrigerator until the expiration date. Opened vials should be labelled with the open date and stored in the refrigerator for up to 28-42 days (depending on the formulation/insulin type) and then discarded. Unopened pens should be stored in the refrigerator until the expiration date. Used pens should be stored at room temperature, but kept away from heat and light, for up to 10-28 days (depending on the formulation/insulin type) and then discarded.
Patient Teaching & Education
See IMSP guidelines for patient teaching in the previous section titled “High Risk Medications and Prevention of Errors.”
Long-Acting Insulin
Insulin glargine (Lantus) and insulin devemir (Levemir) are long-acting insulins given once or twice daily. See Figure 9.14 for an image of a levemir insulin pen.[17]
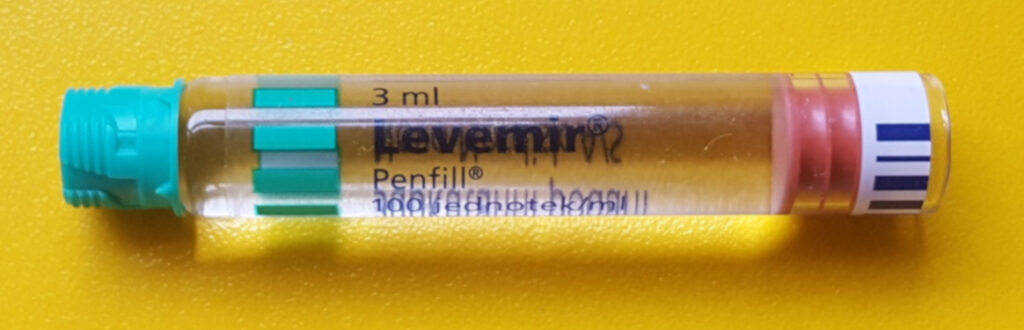
Indications
Long-acting insulins are given once or twice daily. In type 1 diabetics, long-acting insulin should be used concomitantly with rapid- or short-acting insulin at mealtimes.
Mechanism of Action
Insulins lower blood glucose by stimulating peripheral glucose uptake by skeletal muscle and fat and by inhibiting hepatic glucose production.
Specific Administration Considerations
Long-acting insulin has a relatively constant concentration/time profile over 24 hours with no pronounced peak in comparison to NPH insulin. It should only be administered subcutaneously and is available in vials and insulin pens . Inspect insulin visually before use. It should appear clear and colorless; do not use if particulate matter or coloration is seen. Administer subcutaneously into the outer lateral aspect of the upper arm, the abdomen (from below the costal margin to the iliac crest and more than two inches from the umbilicus), the anterior upper thighs, or the buttocks. Rotate injection sites within the same region from one injection to the next to reduce the risk of lipodystrophy.
Patient Teaching & Education
See ISMP guidelines for patient teaching in the previous section titled “High Risk Medications and Prevention of Errors.”
Glucagon
Indications
Glucagon is indicated as a treatment for severe hypoglycemia (low blood sugar), which may occur in patients with diabetes mellitus. Glucagon injection is used for patients who are unable to safely swallow carbohydrates to treat hypoglycemia due to the effects of hypoglycemia or other medical conditions.
Mechanism of Action
Glucagon increases blood glucose concentration during an episode of hypoglycemia. See Figure 9.15 for an image of an emergency glucagon kit.[18]

Specific Administration Considerations
Glucagon may be administered subcutaneously, intramuscularly, or intravenously. Peak glucose levels occur within 13-20 minutes of subcutaneous or IM injection.
Patient Teaching & Education
Patients with type 1 diabetes may have less of an increase in blood glucose levels compared with a stable type 2 patient, so a supplementary carbohydrate should be given as soon as possible, especially to a pediatric patient. [19]
Now let’s take a closer look at the medication grid comparing insulins in Table 9.4a.[20]
Table 9.4a Insulins Medication Grid
| Class/Subclass | Prototypes/Generics | Onset/Peak/Duration | Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|---|
| Rapid-Acting Insulin | insulin lispro (Humalog)
insulin aspart (Novolog) inhaled insulin (Afreeza)
|
Onset: 15-30 minutes
Peak effect: 1-3 hours Duration: 3 - 5 hours |
Administer within 15 minutes before a meal or immediately after a meal
Afrezza is contraindicated in patients with asthma or COPD |
Maintain serum blood glucose in normal range and achieve individualized target level of A1C (often 7%) | Hypoglycemia
Hypokalemia Afrezza can cause acute bronchospasm |
| Short-Acting Insulin | Humulin R
Novolin R |
Onset: 30 minutes
Peak effect: 3 hours Duration: 8 hours |
Administer 30 minutes before a meal | Maintain serum blood glucose in normal range and achieve individualized target level of A1C (often 7%) | Hypoglycemia
Hypokalemia |
| Intermediate-Acting Insulin | Humulin N
Novolin N |
Onset: 1-2 hours
Peak effect: 6 hours (range 2.8-13 hours) Duration: up to 24 hours |
Administer once or twice daily
Only administer subcutaneously Gently roll or invert vial/pen several times to re-suspend the insulin before administration Do not mix with other insulin |
Maintain serum blood glucose in normal range and achieve individualized target level of A1C (often 7%) | Hypoglycemia
Hypokalemia |
| Combination: Intermediate-Acting/Rapid-Acting | Humalog Mix 50/50
Humalog Mix 75/25 Novolog Mix 70/30 *First number is % intermediate-acting insulin, second number is % rapid-acting |
Onset: 15-30 minutes
Peak effect: 50/50: 1-5 hours Duration: 11-22 hours |
Administer twice daily, 15 minutes before a meal or immediately after a meal
Only administer subcutaneously Gently roll or invert vial/pen several times to re-suspend the insulin before administration |
Maintain serum blood glucose in normal range and achieve individualized target level of A1C (often 7%) | Hypoglycemia
Hypokalemia |
| Combination: Intermediate-Acting/Short-Acting | Humulin 70/30
Novolin 70/30 |
Onset: 30-90 minutes
Peak effect: 1.5-6.5 hours Duration: 18-24 hours |
Administer twice daily, 30-45 minutes before a meal
Only administer subcutaneously Gently roll or invert vial/pen several times to re-suspend the insulin before administration Do not mix with other insulin
|
Maintain serum blood glucose in normal range and achieve individualized target level of A1C (often 7%) | Hypoglycemia
Hypokalemia |
| Long-Acting Insulin | insulin glargine (Lantus)
insulin detemir (Levemir) |
Onset: 3-4 hours
Peak effect: none Duration: >24 hours |
Administer once daily (sometimes dose is split and administered twice daily)
Only administer subcutaneously Do not mix with other insulin |
Maintain serum blood glucose in normal range and achieve individualized target level of A1C (often 7%) | Hypoglycemia
Hypokalemia |
| Hyperglycemic | glucagon | May be administered subcutaneously, IM, or IV
Supplementary carbohydrate should be given as soon as possible, especially to a pediatric patient Used to reverse hypoglycemic episode if NPO administration is not appropriate |
Used to reverse hypoglycemic episode if NPO administration is not appropriate | Hyperglycemia |
General adminstration considerations:
- Review orders closely because they may include a standard meal dose, a “sliding scale” dose, and a carb-related dose.
- Always read drug labelling closely as there are several types of dosages and formulations.
- See agency policies and ISMP guidelines for safe administration of insulin.
- When administering with an insulin pen, after inserting the pen count to 5 before removing the needle.
General therapeutic effects:
- Maintain serum blood glucose in normal range and achieve individualized target level of A1C (often 7%)
General side effects:
- Hypoglycemia and hypokalemia
Diabetic Medication: Oral Antihyperglycemics
There are several different classes of oral antihyperglycemic drugs used in conjunction with a healthy diet and exercise for the management of type 2 diabetes. According to the American Diabetes Association, metformin is the preferred initial pharmacologic agent for the treatment of type 2 diabetes.[21]Three of the most commonly used antihyperglycemic classes and prototypes are sulfonylureas (glipizide), biguanide (metformin), and DPP-IV (sitagliptin). The mechanism of action and administration considerations for each of these prototypes are described below.
Glipizide
Mechanism of Action
Glipizide is in the sulfonylurea class of antihyperglycemic medication. The mechanism of action is the stimulation of insulin secretion from the beta cells of pancreatic islet tissue and is thus dependent on functioning beta cells in the pancreatic islets. Peak plasma concentrations occur 1 to 3 hours after a single oral dose.
Specific Administration Considerations
All sulfonylurea drugs are capable of producing severe hypoglycemia. Hypoglycemia may be difficult to recognize in the elderly and in people who are taking beta-adrenergic blocking drugs. Sulfonylurea medications should be given 30 minutes before a meal due to hypoglycemic effects.
Glipizide is contraindicated in type 1 diabetics or for use of diabetic ketoacidosis; insulin should be used to treat this condition. Treatment of patients with glucose 6-phosphate dehydrogenase (G6PD) deficiency with sulfonylurea agents can lead to hemolytic anemia.
The hypoglycemic action of sulfonylureas may be potentiated by certain drugs such as nonsteroidal anti-inflammatory agents and other drugs that are highly protein bound.
Patient Teaching & Education
Patients should take the medication at the same time each day. It is important that patients understand that the medication helps control episodes of hyperglycemia but does not cure diabetes. Patients should be instructed regarding the signs of hyperglycemia and hypoglycemia. The use of sulfonylureas and alcohol may cause a disulfiram-like reaction.
Metformin
Mechanism of Action
Metformin is in the biguanide class of antihyperglycemics. It decreases hepatic glucose production, decreases intestinal absorption of glucose, and improves insulin sensitivity by increasing peripheral glucose uptake and utilization. Unlike sulfonylureas, metformin does not produce hypoglycemia. See Figure 9.16 for an image of a metformin tablet.[22]

Specific Administration Considerations
Metformin hydrochloride should be given in divided doses with meals. The therapeutic goal should be to decrease both fasting plasma glucose and glycosylated hemoglobin levels to near normal by using the lowest effective dose of metformin, either when used as monotherapy or in combination with sulfonylurea or insulin.
Common adverse reactions include diarrhea, nausea/vomiting, weakness, flatulence, indigestion, abdominal discomfort, and headache.
Metformin is contraindicated in patients with kidney disease (e.g., serum creatinine levels ≥1.5 mg/dL [males] or ≥1.4 mg/dL [females]) and should be temporarily discontinued in patients undergoing radiologic studies involving intravascular administration of iodinated contrast materials because use of such products may result in acute alteration of renal function. It is also contraindicated in patients with metabolic acidosis.
Lactic acidosis is a rare, but serious, metabolic complication that can occur due to metformin accumulation during treatment with metformin; when it occurs, it is fatal in approximately 50% of cases. The risk of lactic acidosis increases with the degree of renal dysfunction and the patient’s age. Metformin should be promptly withheld in the presence of any condition associated with hypoxemia, dehydration, or sepsis. Because impaired hepatic function may significantly limit the ability to clear lactate, metformin should be avoided in patients with hepatic disease. The onset of lactic acidosis often is subtle and accompanied only by nonspecific symptoms such as malaise, myalgias, respiratory distress, increasing somnolence, and nonspecific abdominal distress.
Patient Teaching & Education
Patients should take the medication at the same time each day. It is important that patients understand that the medication helps control episodes of hyperglycemia but does not cure diabetes. Patients should be instructed regarding the signs of hyperglycemia and hypoglycemia. The patient may be at risk for lactic acidosis and should report chills, low blood pressure, muscle pain, or dyspnea immediately to the healthcare provider. The use of medications like metformin can cause a metallic taste in the mouth.
Sitagliptin
Mechanism of Action
Sitagliptin is an orally-active inhibitor of dipeptidyl peptidase-4 (DPP-4) enzyme that slows the inactivation of incretin hormones involved in the regulation of glucose homeostasis and thus, increases insulin release and decreases glucagon levels in the circulation. See Figure 9.17 for an image of sitagliptin.[23]
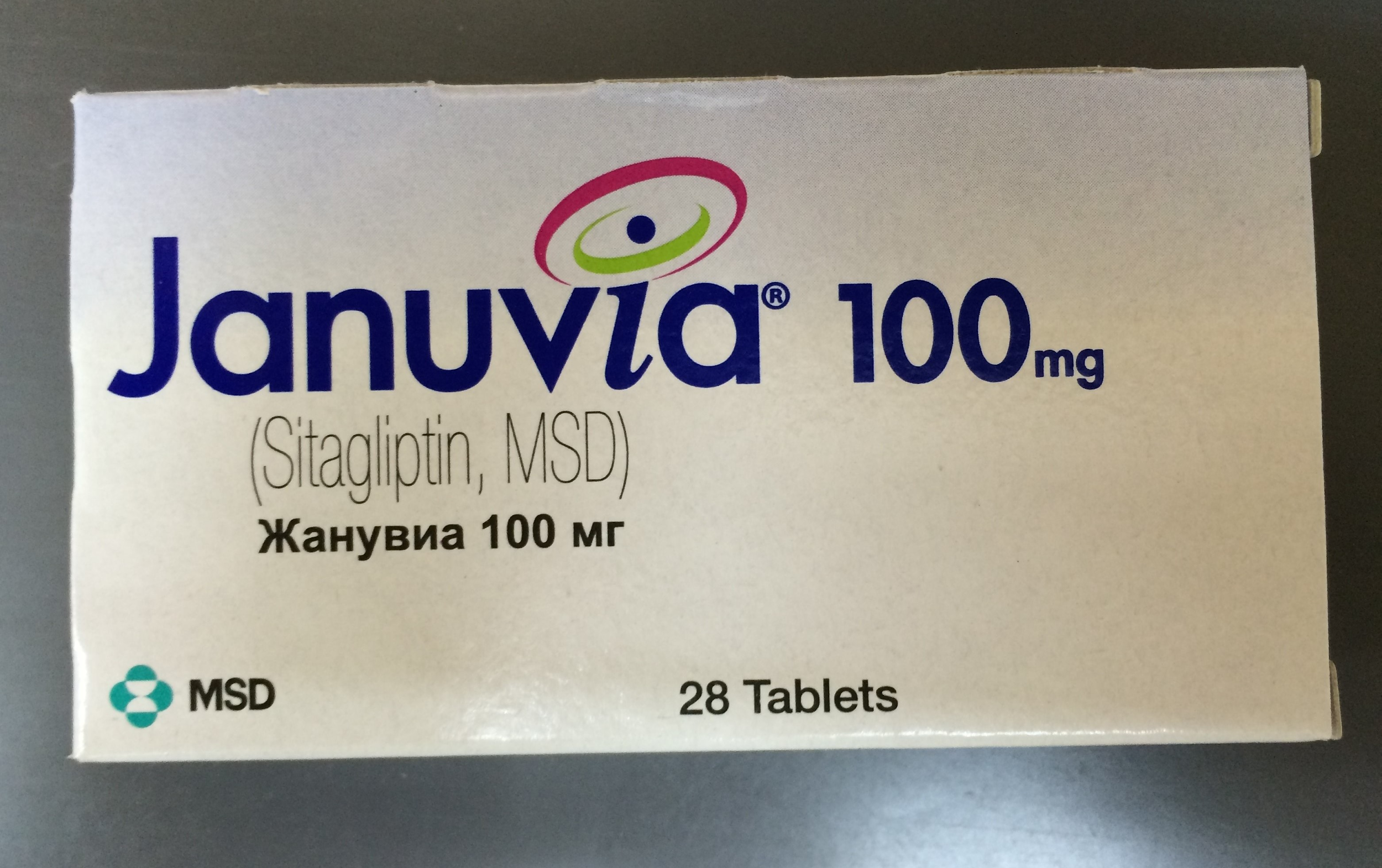
Specific Administration Considerations
Sitagliptin is taken once daily and can be taken with or without food. It can cause hypoglycemia. Dose adjustment should occur for patients with kidney disease depending on their glomerular filtration rate. Report hypersensitivity reactions, blisters/erosions, headache, or symptoms of pancreatitis, heart failure, severe arthralgia, and upper respiratory infection.
Patient Teaching & Education
Patients should take the medication at the same time each day. It is important that patients understand that the medication helps control episodes of hyperglycemia but does not cure diabetes. Patients should be instructed regarding the signs of hyperglycemia and hypoglycemia. Patients should stop taking the medication if symptoms of hypersensitivity occur and follow up immediately with their provider to determine the next course of treatment.
Now let’s take a closer look at the medication grid comparing oral antihyperglycemics in Table 9.4b. [24]
Table 9.4b Medication Grid Comparing Oral Antihyperglycemics
| Class | Prototype | Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Sulfonylureas | glipizide | Time with meals; peak plasma concentrations occur 1 to 3 hours after administration | Reduce fasting blood sugar and glycosylated hemoglobin to near normal | Hypoglycemia; may be potentiated by nonsteroidal anti-inflammatory agents and other drugs that are highly protein bound |
| Biguanide | metformin | Contraindicated in renal and hepatic disease
Should be temporarily discontinued in patients undergoing radiologic studies involving intravascular administration of iodinated contrast materials |
Reduce fasting blood sugar and glycosylated hemoglobin to near normal | Stop immediately if signs of lactic acidosis or any condition associated with hypoxemia, dehydration, or sepsis occurs
Common adverse effects: diarrhea, nausea/vomiting, weakness, flatulence, indigestion, abdominal discomfort, and headache |
| DPP-IV inhibitor | sitagliptin | Can be given with or without food | Reduce fasting blood sugar and glycosylated hemoglobin to near norm | Hypoglycemia
Report hypersensitivity reactions, blisters/erosions, headache, or symptoms of pancreatitis, heart failure, severe arthralgia, or upper respiratory infection |
Critical Thinking Activity 9.4
A patient with diabetes mellitus type 2 is admitted to the hospital for hip replacement surgery. The nurse reviews the following orders:
Diabetic diet with carb counting
Bedside blood glucose testing before meals and at bedtime with sliding scale Humalog insulin
Sliding scale Humalog insulin based on preprandial glucose level:
- 0-150: No coverage
- 151-175: 2 units
- 176-200: 4 units
- 201-225: 6 units
- 226-250: 8 units
- Over 250: call the provider
Insulin coverage per carbohydrate intake at meals: Humalog 2 units/carb
Metformin 1000 mg twice daily
Humulin-N 20 units at breakfast and at bedtime
Hypoglycemia protocol
- Explain the difference between type 1 and type 2 diabetes.
- The patient states that he usually does not take insulin at home. What is the likely rationale for insulin therapy while hospitalized?
- The patient’s blood sugar before breakfast is 223 and he eats 3 carbs at breakfast. What types and amounts of insulin will the nurse administer?
- The nurse reviews the patient's morning lab results and finds a creatinine of 1.8. She plans to call the provider to discuss the impact of the results on the medications ordered. Which medication may require a dosage adjustment based on these results?
- When the nurse enters the room around 4 p.m., she discovers that the patient has become irritable and is shaky. The nurse performs a bedside blood glucose and obtains a value of 60. What is the nurse’s best response?
- What is the likely cause of the patient’s condition? Explain using the onset and peak actions of the insulin orders.
- On admission, the patient’s A1C level was 10%. What does this lab value indicate?
- The provider states the discharge plan is to initiate Lantus insulin therapy at home, based on the admitting A1C level. What patient teaching should the nurse plan to provide before discharge?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
Thyroid Basics: A&P Review
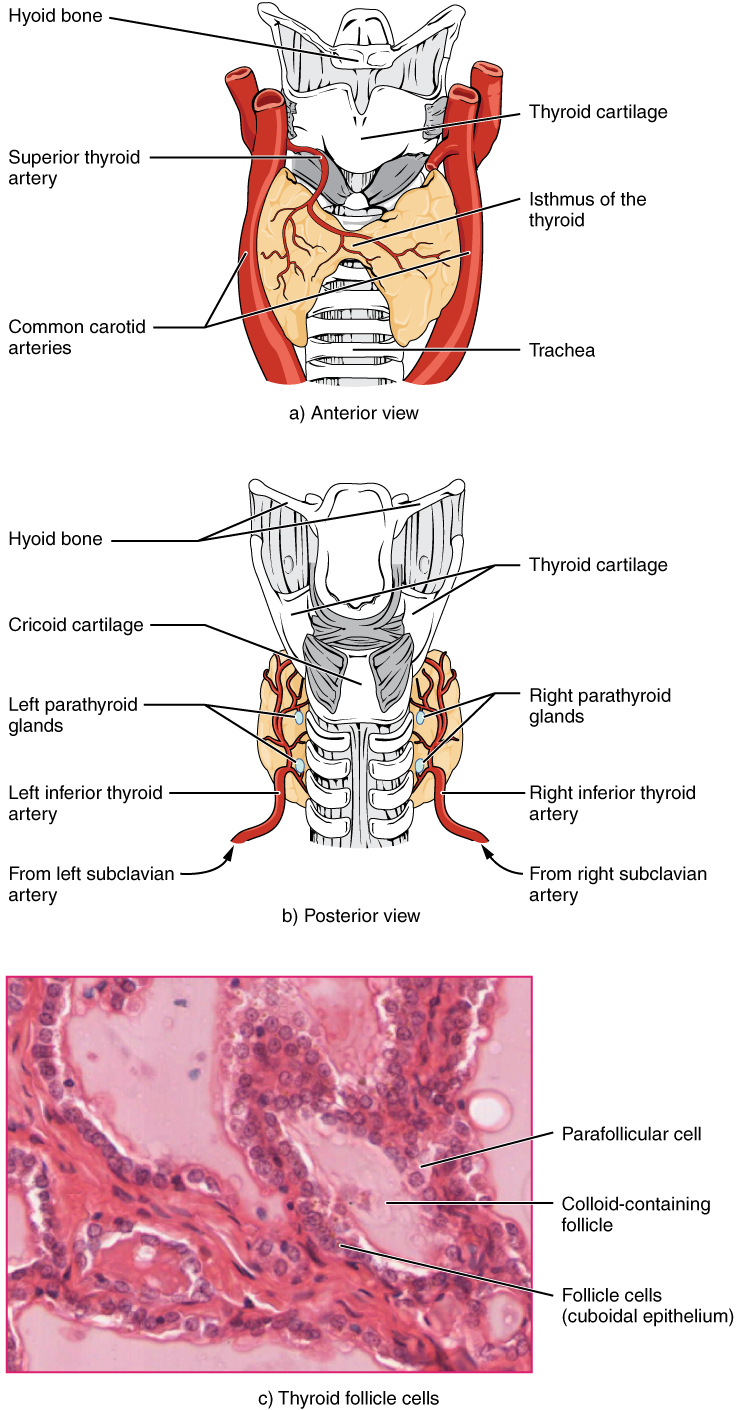
The thyroid is a butterfly-shaped organ located anterior to the trachea, just inferior to the larynx (see Figure 9.18).[25] Each of the thyroid lobes are embedded with parathyroid glands.
Synthesis and Release of Thyroid Hormones
Thyroid hormone production is dependent on the hormone's essential component: iodine. T3 and T4 hormones are produced when iodine attaches to a glycoprotein called thyroglobulin. The following steps outline the hormone's assembly: Binding of TSH to thyroid receptors causes the cells to actively transport iodide ions across their cell membrane from the bloodstream. As a result, the concentration of iodide ions “trapped” in the thyroid cells is many times higher than the concentration in the bloodstream. The iodide ions undergo oxidation (i.e., their negatively charged electrons are removed) and enzymes link the iodine to tyrosine to produce triiodothyronine (T3), a thyroid hormone with three iodines, or thyroxine (T4), a thyroid hormone with four iodines. These hormones remain in the thyroid follicles until TSH stimulates the release of free T3 and T4 into the bloodstream. In the bloodstream, less than one percent of the circulating T3 and T4 remains unbound. This free T3 and T4 can cross the lipid bilayer of cell membranes and be taken up by cells. The remaining 99 percent of circulating T3 and T4 is bound to specialized transport proteins called thyroxine-binding globulins (TBGs), to albumin, or to other plasma proteins. This “packaging” prevents their free diffusion into body cells. When blood levels of T3 and T4 begin to decline, bound T3 and T4 are released from these plasma proteins and readily cross the membrane of target cells. T3 is more potent than T4, and many cells convert T4 to T3 through the removal of an iodine atom.
Regulation of Thyroid Hormone Synthesis
A negative feedback loop controls the regulation of thyroid hormone levels. As shown in Figure 9.19,[26] low blood levels of T3 and T4 stimulate the release of thyrotropin-releasing hormone (TRH) from the hypothalamus, which triggers secretion of TSH from the anterior pituitary. In turn, TSH stimulates the thyroid gland to secrete T3 and T4. The levels of TRH, TSH, T3, and T4 are regulated by a negative feedback system in which increasing levels of T3 and T4 decrease the production and secretion of TSH.
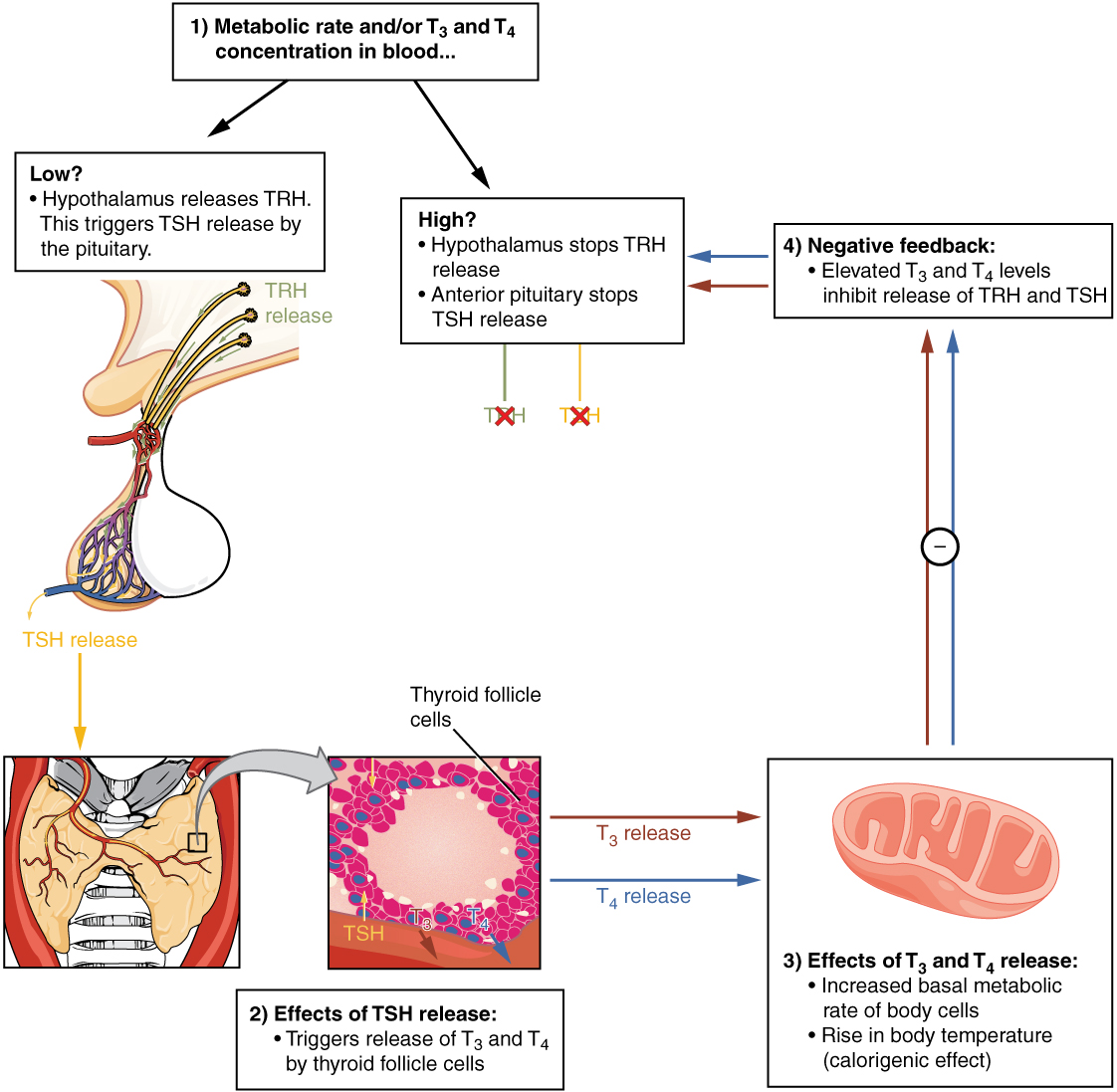
Functions of Thyroid Hormones
The thyroid hormones T3 and T4 are often referred to as metabolic hormones because their levels influence the body’s basal metabolic rate, which is the amount of energy used by the body at rest. When T3 and T4 bind to intracellular receptors located on the mitochondria, they cause an increase in nutrient breakdown and the use of oxygen to produce ATP. In addition, T3 and T4 initiate the transcription of genes involved in glucose oxidation. Although these mechanisms prompt cells to produce more ATP, the process is inefficient, and an abnormally increased level of heat is released as a byproduct of these reactions. This calorigenic effect (calor- = “heat”) raises body temperature.
Adequate levels of thyroid hormones are also required for protein synthesis and for fetal and childhood tissue development and growth. They are especially critical for normal development of the nervous system both in utero and in early childhood, and they continue to support neurological function in adults. Thyroid hormones also have a complex interrelationship with reproductive hormones, and deficiencies can influence libido, fertility, and other aspects of reproductive function. Finally, thyroid hormones increase the body’s sensitivity to catecholamines (epinephrine and norepinephrine) from the adrenal medulla by upregulation of receptors in the blood vessels. When levels of T3 and T4 hormones are excessive, this effect accelerates the heart rate, strengthens the heartbeat, and increases blood pressure. Because thyroid hormones regulate metabolism, heat production, protein synthesis, and many other body functions, thyroid disorders can have severe and widespread consequences.
Disorders of the Thyroid Gland: Iodine Deficiency, Hypothyroidism, and Hyperthyroidism
As discussed above, dietary iodine is required for the synthesis of T3 and T4. For much of the world’s population, foods do not provide adequate levels of iodine because the amount varies according to the level in the soil in which the food was grown, as well as the irrigation and fertilizers used. Marine fish and shrimp tend to have high levels because they concentrate iodine from seawater, but many people in landlocked regions lack access to seafood. Thus, the primary source of dietary iodine in many countries is iodized salt. Fortification of salt with iodine began in the United States in 1924, and international efforts to iodize salt in the world’s poorest nations continue today.
Dietary iodine deficiency can result in the impaired ability to synthesize T3 and T4, leading to a variety of severe disorders. When T3 and T4 cannot be produced, TSH is secreted in increasing amounts. As a result of this hyperstimulation, thyroglobulin and colloid accumulate in the thyroid gland and increase the overall size of the thyroid gland, a condition called a goiter (see Figure 9.20[27]). A goiter is only a visible indication of the deficiency. Other disorders related to iodine deficiency include impaired growth and development, decreased fertility, and prenatal and infant death. Moreover, iodine deficiency is the primary cause of preventable mental retardation worldwide. Neonatal hypothyroidism (cretinism) is characterized by cognitive deficits, short stature, and sometimes deafness and muteness in children and adults born to mothers who were iodine-deficient during pregnancy.

In areas of the world with access to iodized salt, dietary deficiency is rare. Instead, inflammation of the thyroid gland is a common cause of hypothyroidism, or low blood levels of thyroid hormones. Hypothyroidism is a disorder characterized by a low metabolic rate, weight gain, cold extremities, constipation, reduced libido, menstrual irregularities, and reduced mental activity, and requires long-term thyroid hormone replacement therapy. In contrast, hyperthyroidism—an abnormally elevated blood level of thyroid hormones—is often caused by a pituitary or thyroid tumor. In Graves’ disease, the hyperthyroid state results from an autoimmune reaction in which antibodies overstimulate the follicle cells of the thyroid gland. Hyperthyroidism can lead to an increased metabolic rate, excessive body heat and sweating, diarrhea, weight loss, tremors, and increased heart rate. The person’s eyes may bulge (called exophthalmos) as antibodies produce inflammation in the soft tissues of the orbits. The person may also develop a goiter. Hyperthyroidism is often treated by thyroid surgery or with radioactive iodine (RAI) therapy. Patients are asked to follow radiation precautions after RAI treatment to limit radiation exposure to others, especially pregnant women and young children, such as sleeping in a separate bed and flushing the toilet 2-3 times after use. The RAI treatment may take up to several months to have its effect. The end result of thyroid surgery or RAI treatment is often hypothyroidism, which is treated by thyroid hormone replacement therapy.[28]
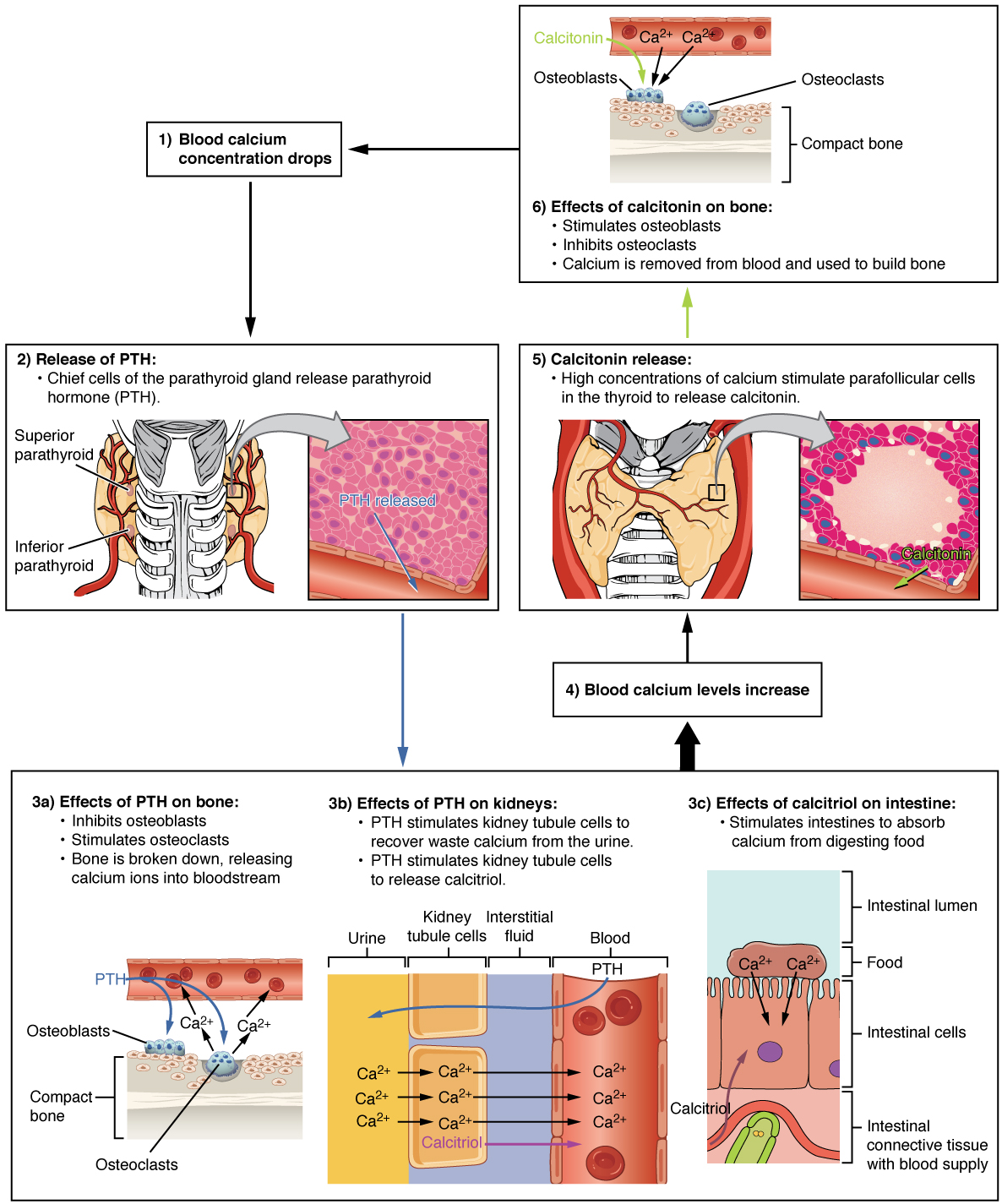
Calcitonin
The thyroid gland also secretes another hormone called calcitonin. Calcitonin is released in response to elevated blood calcium levels. It decreases blood calcium concentrations by:
- Inhibiting the activity of osteoclasts (bone cells that breakdown bone matrix and release calcium into the circulation)
- Decreasing calcium absorption in the intestines
- Increasing calcium loss in the urine
Pharmaceutical preparations of calcitonin are prescribed to reduce osteoclast activity in people with osteoporosis. Osteoporosis is a disease that can be caused by glucocorticoids.
Calcium is critical for many other biological processes. It is a second messenger in many signaling pathways and is essential for muscle contraction, nerve impulse transmission, and blood clotting. Given these roles, it is not surprising that blood calcium levels are tightly regulated by the endocrine system. The parathyroid glands are primarily involved in calcium regulation.
Calcium Regulation: Parathyroid Glands
The parathyroid glands are four tiny, round structures usually embedded in the posterior surface of the thyroid gland (see Figure 9.21).[29] The primary function of the parathyroid glands is to regulate blood calcium levels by producing and secreting parathyroid hormone (PTH) in response to low blood calcium levels.
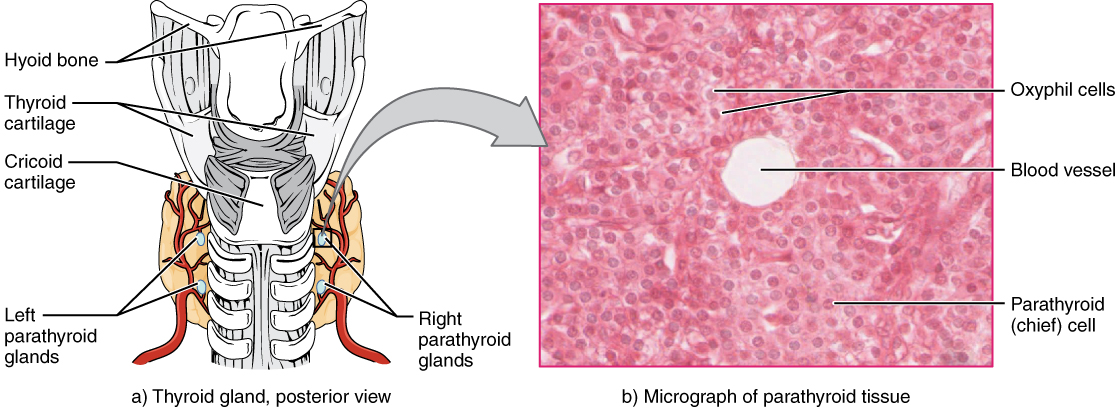
PTH secretion causes the release of calcium from the bones by stimulating osteoclasts that degrade bone and then release calcium into the bloodstream. PTH also inhibits osteoblasts, the cells involved in bone deposition, thereby keeping calcium in the blood. PTH also causes increased reabsorption of calcium (and magnesium) in the kidney and initiates the production of the steroid hormone calcitriol, which is the active form of vitamin D3. Calcitriol then stimulates increased absorption of dietary calcium by the intestines. A negative feedback loop regulates the levels of PTH, with rising blood calcium levels inhibiting further release of PTH. (See Figure 9.22 for an illustration of the role of parathyroid hormone in maintaining blood calcium homeostasis.)[30]
Disorders of the Parathyroid Glands
Abnormally high activity of the parathyroid gland can cause hyperparathyroidism, a disorder caused by an overproduction of PTH that results in excessive degradation of bone and elevated blood levels of calcium, also called hypercalcemia. Hyperparathyroidism can thus significantly decrease bone density, which can lead to spontaneous fractures or deformities. As blood calcium levels rise, cell membrane permeability to sodium is also decreased, and thus the responsiveness of the nervous system is reduced. At the same time, calcium deposits may collect in the body’s tissues and organs, impairing their functioning.
In contrast, abnormally low blood calcium levels may be caused by parathyroid hormone deficiency, called hypoparathyroidism, which may develop following injury or surgery involving the thyroid gland. Low blood calcium increases membrane permeability to sodium, thus increasing the responsiveness of the nervous system, resulting in muscle twitching, cramping, spasms, or convulsions. Severe deficits can paralyze muscles, including those involved in breathing, and can be fatal.
Nursing Considerations
Assessment
When administering thyroid replacement medications, the nurse should plan to monitor TSH levels before and during therapy for effectiveness. Drug interactions may occur with several other medications, so review drug labeling information carefully before administering.
Implementation
Levothyroxine should be administered consistently every morning 30-60 minutes before a meal.
Evaluation
Elevated levels of thyroid hormone can cause cardiac dysrhythmias; immediately report any symptoms of tachycardia, chest pain, or palpitations to the provider.
Thyroid and Osteoporosis Medication Classes
Thyroid Replacement Medication
Indications
Levothyroxine is a thyroid replacement drug used to treat hypothyroidism. See Figure 9.23 for an image of levothyroxine.[31]

Mechanism of Action
Oral levothyroxine sodium is a synthetic T4 hormone that exerts the same physiologic effect as endogenous T4, thereby maintaining normal T4 levels when a deficiency is present.
Specific Administration Considerations
Levothyroxine tablets should be taken with a full glass of water as the tablet may rapidly disintegrate. It should be administered as a single daily dose, on an empty stomach, one-half to one hour before breakfast, and at least 4 hours before or after drugs known to interfere with levothyroxine absorption.
Levothyroxine is contraindicated for patients with hyperthyroidism and adrenal insufficiency until the condition is corrected. Many patients who undergo treatment for hyperthyroidism may develop hypothyroidism. Overtreatment with levothyroxine may cause symptoms of hyperthyroidism with increased heart rate, cardiac wall thickness, and cardiac contractility that may precipitate angina or arrhythmias, particularly in patients with cardiovascular disease and in elderly patients. Levothyroxine therapy in this population should be initiated at lower doses. If cardiac symptoms develop or worsen, the nurse should withhold the medication, contact the health care provider, and anticipate a lower dose prescribed or the medication to be withheld for one week then restarted at a lower dose.
Addition of levothyroxine therapy in patients with diabetes mellitus may worsen glycemic control and result in the need for higher dosages of antidiabetic medication. Carefully monitor glycemic control, especially when thyroid therapy is started, changed, or discontinued.
Levothyroxine increases the response to oral anticoagulant therapy. Therefore, a decrease in the dose of anticoagulant may be warranted with correction of the hypothyroid state or when the levothyroxine dose is increased. Closely monitor INR results and anticipate dosage adjustments.
Levothyroxine can affect, or be affected by, several other medications, so carefully read drug label information when therapy is initiated.
Pregnancy: There are risks to the mother and fetus associated with untreated hypothyroidism in pregnancy. Because TSH levels may increase during pregnancy, TSH should be monitored and levothyroxine dosage may require adjustment during pregnancy.[32]
Patient Teaching & Education
Patients should take thyroid replacement medications at the same time each day. Patients should be aware that thyroid replacement medications do not cure hypothyroidism and therapy is lifelong. Patients should notify their healthcare provider if they experience signs of headache, diarrhea, sweating, or heat intolerance. Medications should be spaced four hours apart from medications like antacid, iron, or calcium supplements. Patients will be followed closely by their healthcare provider regarding their response to medication therapy and serum thyroid levels will be taken.[33]
Antithyroid Medication
Indications
Propylthiouracil (PTU) is an antithyroid medication used to treat hyperthyroidism or to ameliorate symptoms of hyperthyroidism in preparation for thyroidectomy or radioactive iodine therapy.
Mechanism of Action
Propylthiouracil inhibits the synthesis of thyroid hormones.
Specific Administration Considerations
Propylthiouracil is administered orally. The total daily dosage is usually given in 3 equal doses at approximately 8-hour intervals. Propylthiouracil can cause hypothyroidism necessitating routine monitoring of TSH and free T4 levels, with adjustments in dosing to maintain a euthyroid state.
Liver injury resulting in liver failure, liver transplantation, or death has been reported. Patients should be instructed to report any symptoms of hepatic dysfunction (anorexia, pruritus, and right upper quadrant pain), particularly in the first six months of therapy.
Agranulocytosis is a potentially life-threatening side effect of propylthiouracil therapy. Agranulocytosis typically occurs within the first 3 months of therapy. Patients should be instructed to immediately report any symptoms suggestive of agranulocytosis, such as fever or sore throat.
Cases of vasculitis resulting in severe complications and death have been reported in patients receiving propylthiouracil therapy. If vasculitis is suspected, discontinue therapy and initiate appropriate intervention.
Pregnancy: Propylthiouracil crosses the placenta and can cause fetal liver failure, goiter, and cretinism if administered to a pregnant woman.
Patient Teaching & Education
Patients should take the medication as directed at regular dosing intervals. They should monitor their weight 2-3 times per week. Additionally, patients should be advised that medications may cause drowsiness, and they should report any signs of sore throat, fever, headache, jaundice, bleeding, or bruising.
Osteoporosis Medication: Calcitonin
Indications
Calcitonin is used to treat osteoporosis.
Mechanism of Action
Calcitonin is a calcitonin receptor agonist. Calcitonin is released by the thyroid gland. It acts primarily on bone and also has effects on the kidneys and the gastrointestinal tract.
Specific Administration Considerations
Calcitonin is administered via nasal spray with one spray in one side of the nose daily. See Figure 9.24 for an image of calcitonin nasal spray.[34] The nasal spray pump should be primed before the first administration. Unopened calcitonin can be stored in the refrigerator until opened, but should not be refrigerated between doses. Opened bottles stored at room temperature should be discarded after 30 days of initial dose.
Adverse effects include serious hypersensitivity reactions (bronchospasm, swelling of the tongue or throat, anaphylaxis and anaphylactic shock), hypocalcemia, nasal mucosa adverse events, and malignancy.
Pregnancy: Calcitonin should not be used during pregnancy.
Patient Teaching & Education
Patients should be advised to take medications as directed. They should report any signs of hypercalcemia or an allergic response. Patients should receive instruction on the process of self-injection. They should also be advised that they may experience flushing and warmth following injection. Post-menopausal women should adhere to a diet high in calcium and vitamin D, and should be educated regarding the importance of exercise for reversing bone loss.[35]
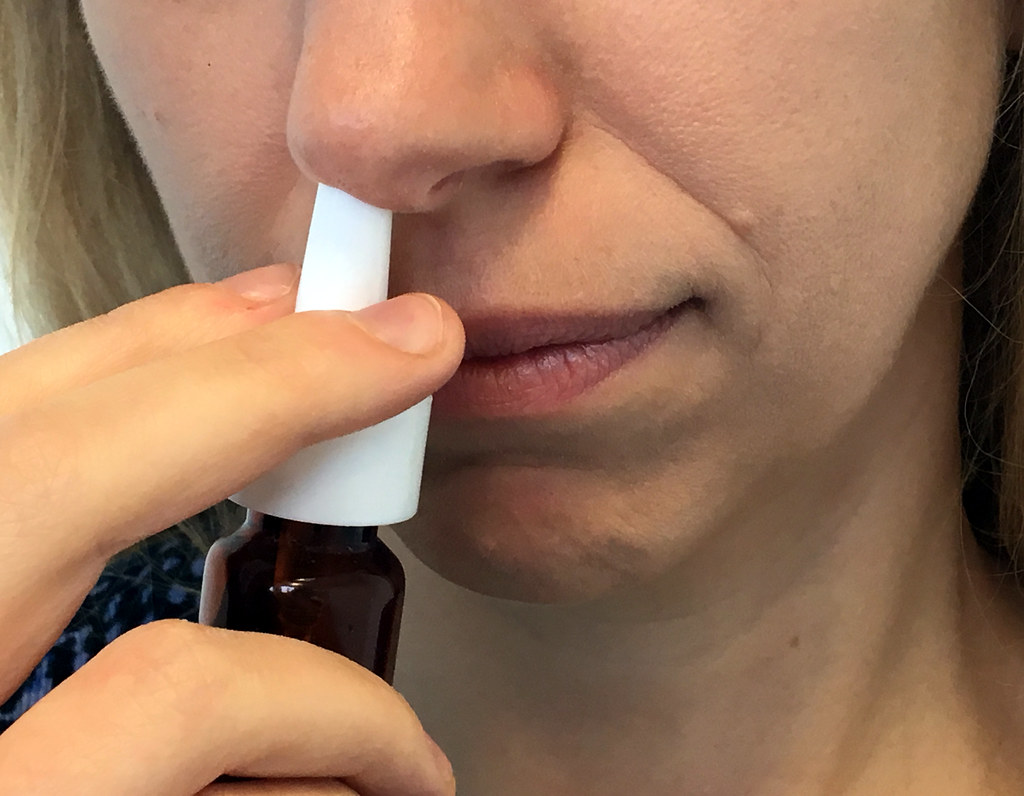
Indications
Alendronate is used for the prevention and treatment of osteoporosis in postmenopausal women, to increase bone mass in men with osteoporosis, and for glucocorticoid-induced osteoporosis.
Mechanism of Action
Alendronate is a bisphosphonate that inhibits osteoclast-mediated bone resorption. By preventing the breakdown of bone and enhancing the formation of new bone, alendronate assists in reversing bone loss and decreases the risk of fractures.
Specific Administration Considerations
Check dosages carefully because some formulations are administered daily, whereas others are administered one weekly. Alendronate should be taken upon arising for the day, but should be administered at least one-half hour before the first food, beverage, or medication of the day with plain water only. Other beverages (including mineral water), food, and some medications are likely to reduce the absorption of alendronate. Patients should not lie down for at least 30 minutes and until after their first food of the day. Patients may also require calcium and vitamin D supplementation, especially if concurrently taking glucocorticoids.
Alendronate is contraindicated in the following conditions: pregnancy, hypocalcemia, the inability to sit or stand for 30 minutes after swallowing, esophageal abnormalities that delay emptying, and patients at risk for aspiration. Alendronate is not recommended for patients with kidney disease with creatinine clearance less than 35 mL/min.
Discontinue alendronate if severe musculoskeletal pain occurs. A bone mineral density measurement should be made at the initiation of therapy and repeated after 6 to 12 months of combined alendronate and glucocorticoid treatment.
Patient Teaching & Education
Patients should take medication as directed at the same time each day, first thing in the morning. Patients should remain upright after they take medication for 30 minutes to minimize stomach and esophageal irritation. Patients should eat a balanced diet and may seek advice from the healthcare provider regarding supplementation with calcium and vitamin D. Patients should participate in regular exercise to help increase bone strength.[36]
Now let’s take a closer look at the medication grid comparing thyroid and osteoporosis medications in Table 9.5.[37] Medication grids are intended to assist students to learn key points about each medication. Because information about medication is constantly changing, nurses should always consult evidence-based resources to review current recommendations before administering specific medication. Basic information related to each class of medication is outlined below. Detailed information on a specific medication can be found for free at Daily Med at https://dailymed.nlm.nih.gov/dailymed/index.cfm. On the home page, enter the drug name in the search bar to read more about the medication. Prototype/generic medications listed in the grids below are also hyperlinked directly to a Daily Med page.
Table 9.5. Medication Grid Comparing Thyroid and Osteoporosis Medications
| Class | Prototype/Generic | Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Thyroid replacement | levothyroxine | Take levothyroxine sodium tablets with a full glass of water as the tablet may rapidly disintegrate
Administer levothyroxine as a single daily dose, on an empty stomach, one-half to one hour before breakfast Administer levothyroxine at least 4 hours before or after drugs known to interfere with levothyroxine sodium tablets absorption Anticipate lower dosages in elderly patients with pre-existing cardiac disease May interact with several medications so read drug label thoroughly on initial administration for potential effects |
Increases T4 levels in hypothyroidism | Hypersensitivity reactions
Cardiac dysrhythmias |
| Antithyroid | propylthiouracil | Usually administered every 8 hours
May cause hypothyroidism so TSH and T4 levels should be monitored If a patient becomes pregnant, immediately notify health care provider because it can cause fetal harm |
Inhibit production of T4 | Hypothyroidism
Liver failure Agranulocytosis Vasculitis Fetal harm |
| Calcium regulator | calcitonin | Administer nasal spray with one spray in one side of the nose daily
Contraindicated during pregnancy Discard unrefrigerated bottle after 30 days of opening May store unopened bottles in refrigerator until expiration date |
Treats osteoporosis | Serious hypersensitivity reactions (bronchospasm, swelling of the tongue or throat, anaphylaxis, and anaphylactic shock)
Hypocalcemia Nasal mucosa adverse effects Malignancy |
| Bisphosphonates | alendronate | Administered upon arising and at least one-half hour before the first food, beverage, or medication of the day with plain water only
The patient should sit or stand for 30 minutes after administration Contraindicated in pregnancy, hypocalcemia, and kidney disease Concurrent calcium and vitamin D supplements may be required |
Enhances bone mineral density in osteoporosis | Upper GI tract adverse events
Severe musculoskeletal pain Risk of osteonecrosis of the jaw |
Critical Thinking Activity 9.5
A patient has been diagnosed with hypothyroidism and receives a prescription for levothyroxine.
What patient education should the nurse provide regarding taking this medication?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
Interactive Activity
Interactive Activity
Interactive Activity
Interactive Activity
You may never have thought of it this way, but when you send a text message to two friends to meet you at a restaurant at six, you're sending digital signals that you hope will affect their behavior—even though they are some distance away. Similarly, certain cells send chemical signals to other cells in the body that influence their behavior. This long-distance intercellular communication, coordination, and control are critical for homeostasis, and it is the fundamental function of the endocrine system.
Whereas the nervous system uses neurotransmitters to communicate, the endocrine system uses hormones for chemical signaling. These hormone signals are sent by the endocrine organs. Hormones are transported primarily via the bloodstream throughout the body, where they bind to receptors on target cells, inducing a characteristic response. Some of the glands in the endocrine system include the pituitary, thyroid, parathyroid, adrenal, and pineal glands. See Figure 9.1 for an illustration of the endocrine system.[38] Some of these glands have both endocrine and nonendocrine functions. For example, the pancreas contains cells that function in digestion, as well as cells that secrete the hormones insulin and glucagon, which regulate blood glucose levels.[39]
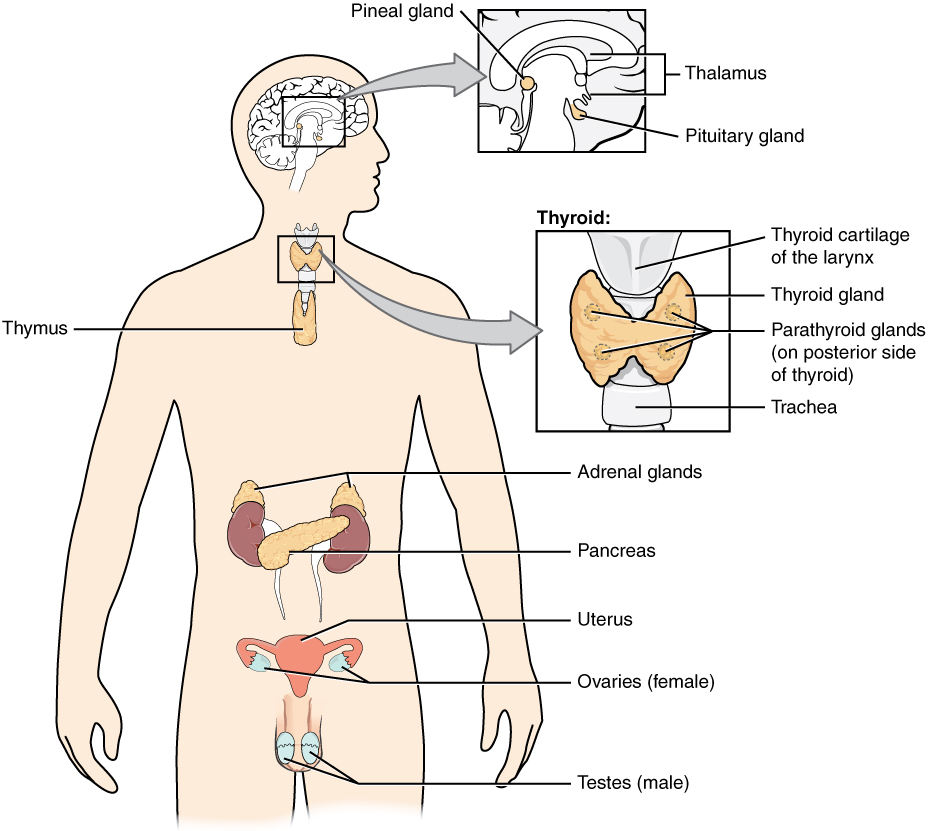
This module will focus on medications that affect three major endocrine glands and their hormones: the adrenal glands, the pancreas, and the thyroid. See Table 9.1 for a list of hormones associated with each of these glands and their effects.[40]
Table 9.1. Hormones Associated with Adrenal Gland, Pancreas, and Thyroid and Their Effects
| Endocrine gland | Hormone | Effect |
|---|---|---|
| Adrenal (cortex) | Aldosterone | Increases blood Na+ levels |
| Adrenal (cortex) | Cortisol | Increases blood sugar levels |
| Adrenal (medulla) | Epinephrine and Norepinephrine | Stimulates fight-or-flight response |
| Pancreas | Insulin | Reduces blood glucose levels |
| Pancreas | Glucagon | Increases blood glucose levels |
| Thyroid | Thyroxine (T4), triiodothyronine (T3) | Stimulates basal metabolic rate |
| Thyroid | Calcitonin | Reduces blood Ca+ levels |
Regulation of Hormone Secretion
To prevent abnormal hormone levels and a potential disease state, hormone levels must be tightly controlled. Feedback loops govern the initiation and maintenance of hormone secretion in response to various stimuli.
The most common method of hormone regulation is the negative feedback loop. Negative feedback is characterized by the inhibition of further secretion of a hormone in response to adequate levels of that hormone. This allows blood levels of the hormone to be regulated within a narrow range. An example of a negative feedback loop is the release of glucocorticoid hormones from the adrenal glands, as directed by the hypothalamus and pituitary gland. As glucocorticoid concentrations in the blood rise, the hypothalamus and pituitary gland reduce their signaling to the adrenal glands to prevent additional glucocorticoid secretion.[41] See Figure 9.2 for an illustration of a negative feedback loop.[42]
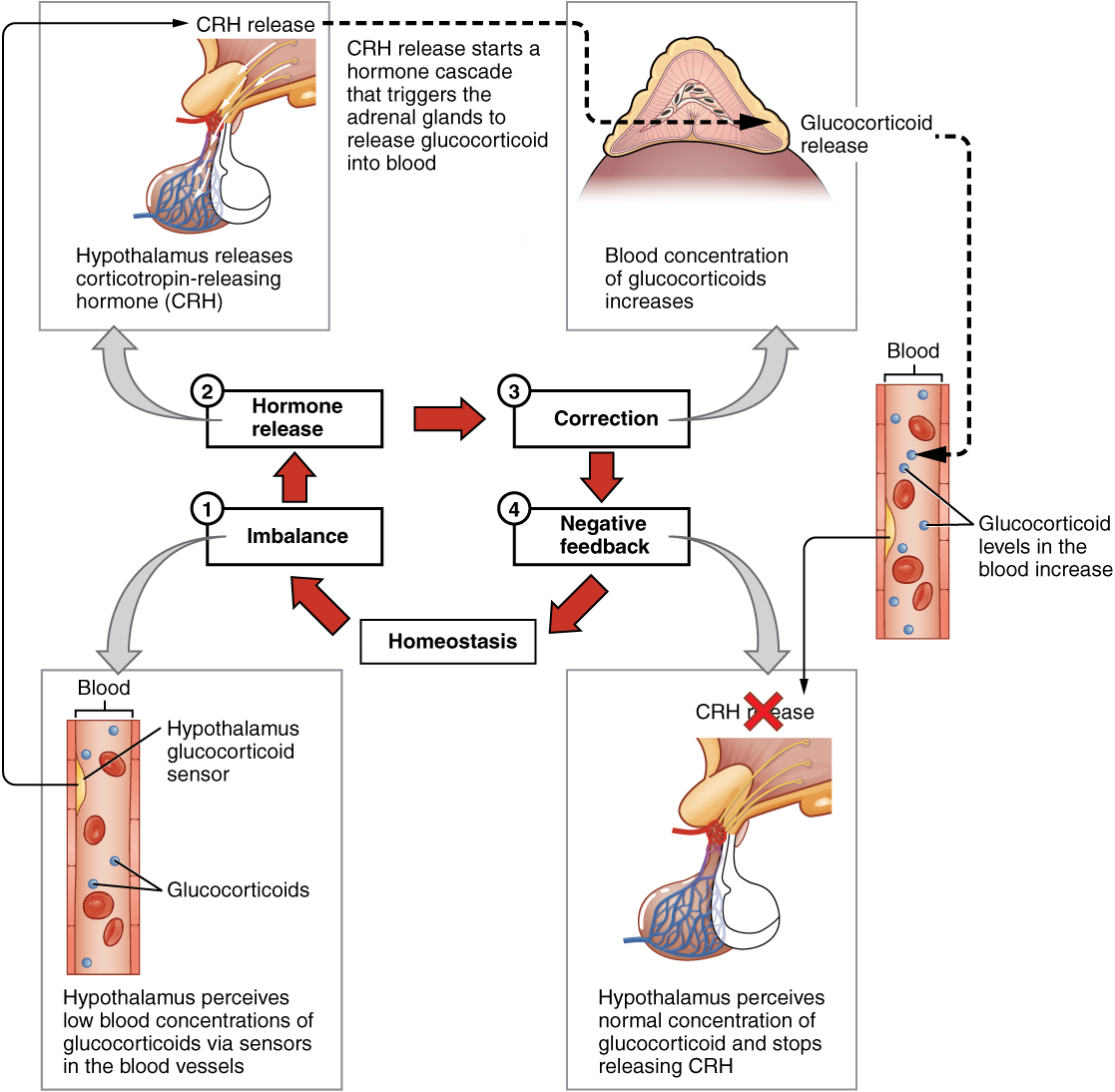
Endocrine Gland Stimuli
Endocrine glands can be stimulated by humoral stimuli, by stimulation of another hormone, or by neural stimuli. Humoral stimuli are changes in blood levels of non-hormone chemicals that cause the release or inhibition of a hormone to maintain homeostasis. For example, osmoreceptors in the hypothalamus detect changes in blood osmolarity (the concentration of solutes in the blood plasma). If blood osmolarity is too high, meaning that the blood is not dilute enough, osmoreceptors signal the hypothalamus to release ADH (antidiuretic hormone). ADH causes the kidneys to reabsorb more water and reduce the volume of urine produced. This reabsorption causes a reduction of the osmolarity of the blood by diluting the blood to the appropriate level. Another example of humoral stimuli is the regulation of blood glucose. High blood glucose levels cause the release of insulin from the pancreas, which increases glucose uptake by cells and liver storage of glucose as glycogen.
An endocrine gland may also secrete a hormone in response to the presence of another hormone produced by a different endocrine gland. For example, the thyroid gland secretes T4 into the bloodstream when triggered by thyroid-stimulating hormone (TSH) that is released from the anterior pituitary gland.
In addition to these chemical signals, hormones can also be released in response to neural stimuli. An example of neural stimuli is the activation of the fight-or-flight response by the sympathetic nervous system. When an individual perceives danger, sympathetic neurons signal the adrenal glands to secrete norepinephrine and epinephrine. The two hormones dilate blood vessels, increase the heart and respiratory rate, and suppress the digestive and immune systems. These responses boost the body's transport of oxygen to the brain and muscles, thereby improving the body's ability to fight or flee.[43]
The Hypothalamus–Pituitary Complex
The hypothalamus–pituitary complex can be thought of as the "command center" of the endocrine system. This complex secretes several hormones that directly produce responses in target tissues, as well as hormones that regulate the synthesis and secretion of hormones of other glands. In addition, the hypothalamus–pituitary complex coordinates the messages of the endocrine and nervous systems. In many cases, a stimulus received by the nervous system must pass through the hypothalamus–pituitary complex to be translated into hormones that can initiate a response. See Figure 9.3 for an illustration of the hypothalamus–pituitary complex.[44] The hypothalamus connects to the pituitary gland by the stalk-like infundibulum. The pituitary gland consists of an anterior and posterior lobe, with each lobe secreting different hormones in response to signals from the hypothalamus.
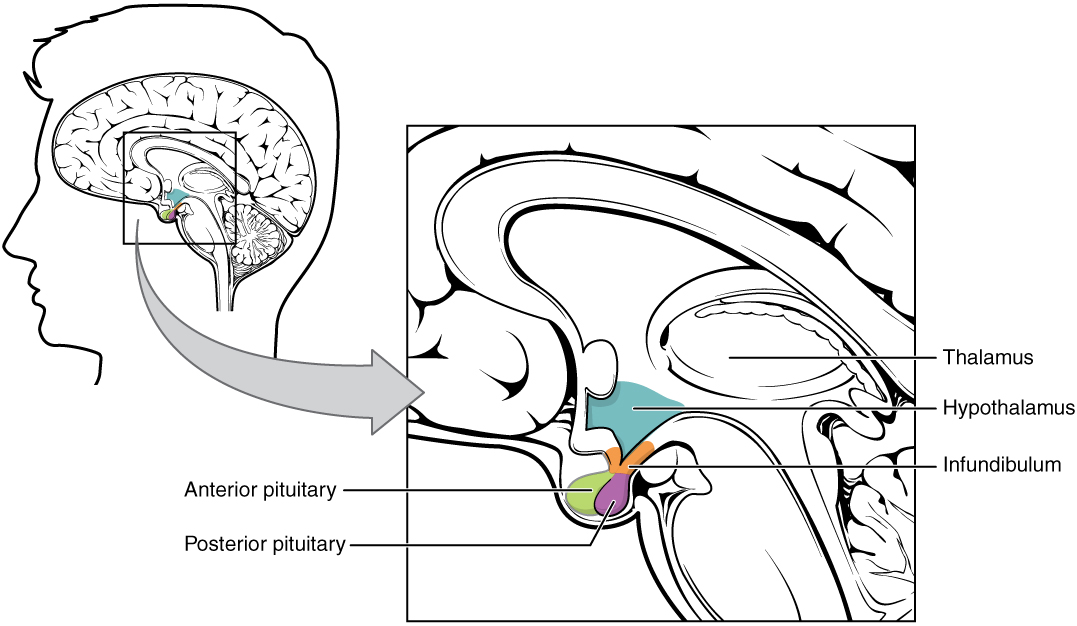
Posterior Pituitary
The posterior pituitary gland does not produce hormones, but stores and secretes two hormones produced by the hypothalamus: oxytocin and antidiuretic hormone (ADH).
Antidiuretic Hormone (ADH)
Blood osmolarity, the concentration of sodium ions and other solutes, is constantly monitored by osmoreceptors in the hypothalamus. Blood osmolarity may change in response to the consumption of certain foods and fluids, as well as in response to disease, injury, medications, or other factors. In response to high blood osmolarity, which can occur during dehydration or following a very salty meal, the osmoreceptors signal the posterior pituitary to release antidiuretic hormone (ADH). Its effect is to cause increased water reabsorption by the kidneys. As more water is reabsorbed by the kidneys, a greater amount of water is returned to the blood, thus causing a decrease in blood osmolarity. The release of ADH is controlled by a negative feedback loop. As blood osmolarity decreases, the hypothalamic osmoreceptors sense the change and prompt a corresponding decrease in the secretion of ADH. As a result, less water is reabsorbed by the kidneys.
Drugs can also affect the secretion of ADH or imitate its effects. For example, alcohol consumption inhibits the release of ADH, resulting in increased urine production that can eventually lead to dehydration and a hangover. Vasopressin is a synthetic ADH medication used to treat very low blood pressure. It is called vasopressin because in very high concentrations it also causes constriction of blood vessels in addition to the retention of water. Vasopressin is also used to treat a disease called diabetes insipidus (DI) that causes dehydration due to an underproduction of ADH. [45]
Anterior Pituitary
In contrast to the posterior pituitary, the anterior pituitary does manufacture hormones. However, the secretion of hormones from the anterior pituitary is regulated by two classes of hormones secreted by the hypothalamus called releasing hormones. Releasing hormones then stimulate the secretion of hormones from the anterior pituitary (see Figure 9.4[46]). The anterior pituitary produces seven hormones. These are the growth hormone (GH), thyroid-stimulating hormone (TSH), adrenocorticotropic hormone (ACTH), follicle-stimulating hormone (FSH), luteinizing hormone (LH), beta endorphin, and prolactin. Of the hormones of the anterior pituitary, TSH, ACTH, FSH, and LH are collectively referred to as tropic hormones (trope- = "turning") because they turn on or off the function of other endocrine glands. This module will focus on the effects of TSH and ACTH.
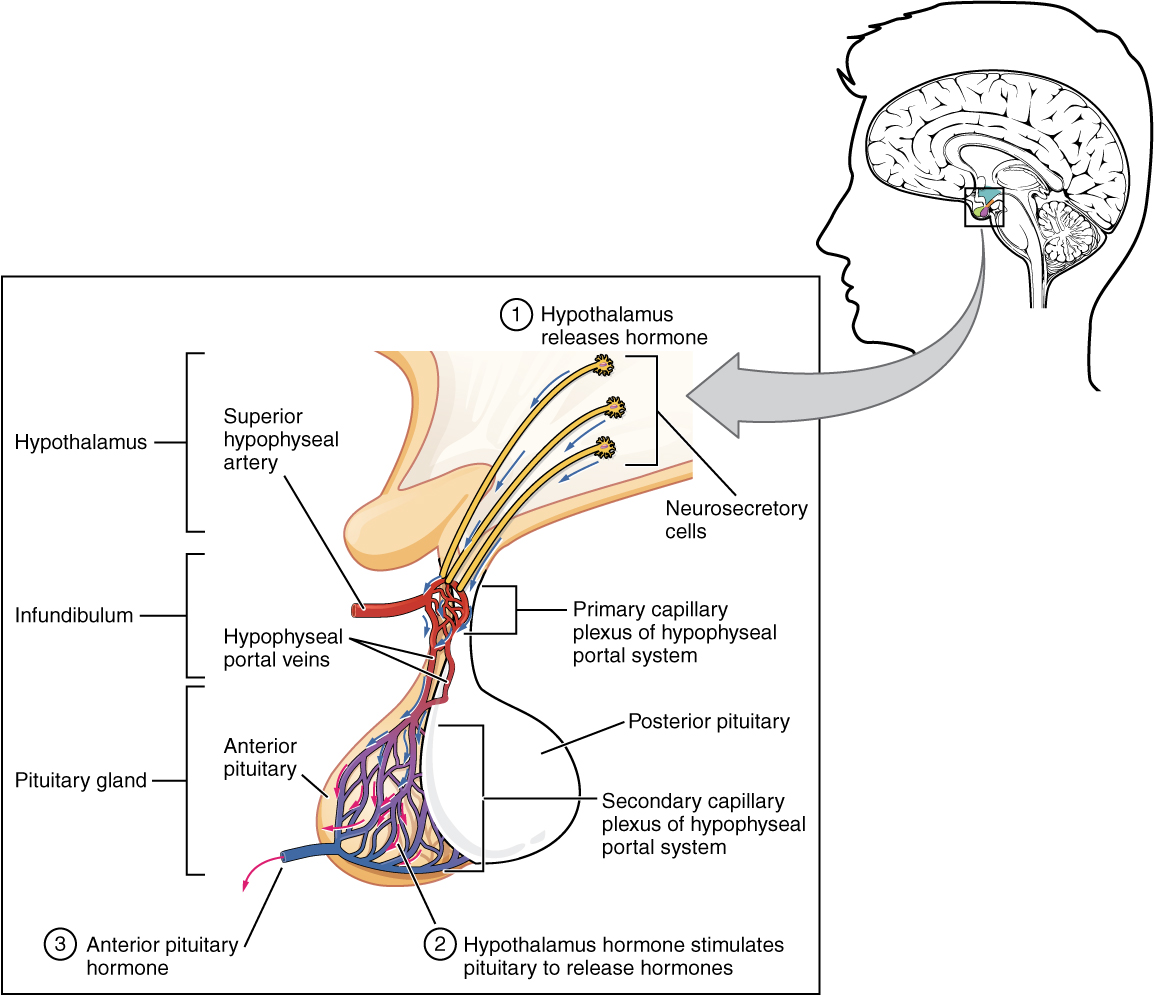
Thyroid-Stimulating Hormone (TSH)
The activity of the thyroid gland is regulated by the thyroid-stimulating hormone (TSH). TSH is released from the anterior pituitary in response to the thyrotropin-releasing hormone (TRH) from the hypothalamus and triggers the secretion of thyroid hormones by the thyroid gland. In a classic negative feedback loop, elevated levels of thyroid hormones in the bloodstream then trigger a drop in production of TRH and subsequently, the production of TSH. TSH is further discussed in the "Thyroid" submodule.
Adrenocorticotropic Hormone (ACTH)
The adrenocorticotropic hormone (ACTH) is released from the anterior pituitary in response to the corticotropin-releasing hormone (CRH) from the hypothalamus. ACTH then stimulates the adrenal cortex to secrete corticosteroid hormones such as cortisol. A variety of stressors can also influence the release of ACTH, and the role of ACTH in the stress response is discussed under the "Adrenal" submodule.[47]
Interactive Activity
Now that we have reviewed antimicrobial basics and administration considerations, we will take a closer look at specific antimicrobial classes and administration considerations, therapeutic effects, adverse effects, and specific teaching needed for each class of antimicrobials. But before we do that, let's reexamine the importance of the nursing process in guiding the nurse who administers antimicrobial medications. The nursing process consists of assessment, diagnosis, outcome identification, planning, implementation of interventions, and evaluation. For more information about the nursing process, refer to the Chapter 2 sub-module on "Ethical and Professional Foundations of Safe Medication Administration by Nurses." Because diagnosis, outcome identification, and planning are specifically tailored to the individual patient, we will broadly discuss considerations related to assessment, implementation of interventions, and evaluation when administering antimicrobials.
Nursing Process: Assessment
Although there are numerous details to consider when administering medications, it is important to always first think more broadly about what you are giving and why. As a nurse who is administering an antimicrobial, you must remember some important broad considerations.
First, let's think of the WHY?
Antimicrobials are given to prevent or treat infection. If a patient is prescribed an antimicrobial, an important piece of the nursing assessment should be to look for signs and symptoms of infection. The nurse should always know WHY the patient is receiving an antimicrobial to evaluate if the patient is improving or deteriorating. Remember, the nurse must assess how this medication is working, and having pre-administration assessment information is an important part of this process. Typical data that a nurse collects at the start of a shift include a baseline temperature, heart rate, blood pressure, and white blood cell count. Focused assessments are then made based on the type of infection. For example, if it is a wound infection, the wound should be assessed. If it is a respiratory infection, the nurse should assess the patient's lung sounds. If a patient has a urinary tract infection (UTI), the urine and symptoms related to a UTI should be assessed. Additionally, whenever a patient has an infection, it is important to continually monitor for the development of sepsis, a life-threatening condition caused by severe infection. Early signs of sepsis include new onset confusion, elevated heart rate, decreased blood pressure, increased respiratory rate, and elevated fever.
Additional baseline information to collect prior to the administration of any new medication order includes a patient history, current medication use including herbals or other supplements, and history of allergy or previous adverse response. Many patients with an allergy to one type of antimicrobial agent may experience cross-reactivity to other classes. This information should be appropriately communicated to the prescribing provider prior to the administration of any antimicrobial medication.
Nursing Process: Implementation of Interventions
With administration of the antimicrobial medication, it is important for the nurse to anticipate any additional interventions associated with the medications. For example, antimicrobials often cause gastrointestinal upset (GI) such as nausea, diarrhea, etc. The patient should be educated about these potential side effects, and proper interventions should be taken to minimize these occurrences. For example, the nurse may instruct the patient to take certain antimicrobials with food to diminish the chance of GI upset, whereas other medications should be taken on an empty stomach for optimal absorption.
Hypersensitivity/allergic reactions are always a potential adverse reaction, especially when administering the first dose of a new antibiotic, and the nurse should monitor for these symptoms closely and respond appropriately by immediately notifying the prescriber. Hypersensitivity reactions are immune responses that are exaggerated or inappropriate to an antigen and can range from itching to anaphylaxis. Anaphylaxis is a medical emergency that can cause life-threatening respiratory failure. Early signs of anaphylaxis include, but are not limited to, hives and itching, the feeling of a swollen tongue or throat, shortness of breath, dizziness, and low blood pressure.
Nursing Process: Evaluation
Finally, it is important to always evaluate the patient's response to a medication. With antimicrobial medications, the nurse should assess for absence of or decreasing signs of infection, indicating the patient is improving. It is important to document these findings to reflect the patient's trended response.
Additionally, it is also important for the nurse to promptly identify and communicate signs of worsening infection to the provider. For example, increasing white blood cell count, temperature, heart rate, and respiratory rate may indicate that the patient's body is experiencing a life-threatening response to the infection. These signs of worsening clinical assessment require prompt intervention to prevent further clinical deterioration. Additionally, patients receiving antibiotics should be closely monitored for developing a complication called "C-diff," resulting in frequent, foul-smelling stools. C-diff requires the implementation of modified contact precautions, including the use of soap and water, not hand sanitizer, as well as antibiotic therapy. [48]
