3.3 Administration Considerations
The administration of antimicrobial drug therapy involves special considerations to ensure that the therapeutic drug effect is achieved while maintaining patient safety and minimizing complications.
Let’s consider some of the variables that may impact antimicrobial administration:
Half-Life
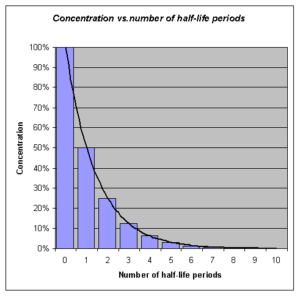
Many antimicrobial medications are administered to ensure a certain therapeutic level of medication remains in the bloodstream and may require interval or repeated dosing throughout the day. For example, the half-life, or rate at which 50% of a drug is eliminated from the plasma, can vary significantly between drugs. Some drugs have a short half-life of only 1 hour and must be given multiple times a day, but other drugs have half-lives exceeding 12 hours and can be given as a single dose every 24 hours. Although a longer half-life can be considered an advantage for an antibacterial when it comes to convenient dosing intervals, the longer half-life can also be a concern for a drug with serious side effects. Medications that have longer half-life and more concerning side effects will exert these side effects over a longer period of time.
See Figure 3.6[1] for an illustration of half-lives and the time it takes for a medication to be eliminated from the bloodstream.
Lifespan Considerations
A majority of medications are calculated specifically based on the patient’s size, weight, and renal function. Patient age and size are especially vital in pediatric patients. A child’s stage of development and the size of their internal organs will greatly impact how the body absorbs, digests, metabolizes, and eliminates medications.
Liver & Renal Function
Additionally, there are many antimicrobial medications that will require tailored dosing based on individual patient response and the potential impact of the medication on the patient’s liver and renal function. For more information about the effects of liver and renal function on medications, refer to Chapter 1 regarding metabolism and excretion. Often times, pharmacists and providers will collect drug peak and trough drug blood levels to determine how an individual patient’s body is responding to an antimicrobial. Follow-up interval dosing is then prescribed based on these blood levels. This is especially important for older adults or those with known liver/renal impairment. Individuals with diminished liver and renal function are more prone to drug toxicity because of the reduced ability of the body to metabolize or clear medications from the body. For more information about peak and trough levels, refer to Chapter 1 regarding medication safety. [2]
Dose Dependency/Time Dependency
The goal of antimicrobial therapy is to select an optimal dosage that will result in clinical cure, while reducing the patient complications or significant side effects. Many medications may be dose dependent. This means that there is a more significant killing of the bacterial with increasing levels of the antibiotic. For example, fluroquinolones are dose-dependent medications with the treatment goal to optimize the amount of the drug. Other medications are time dependent. Time-dependent medications have optimal bacterial killing effect at lower doses over a longer period of time. Time-dependent antimicrobials exert the greatest effect by binding to the microorganism for an extensive length of time. Penicillin is an example of a time-dependent medication where the goal is to optimize the duration of exposure.[3]
Route
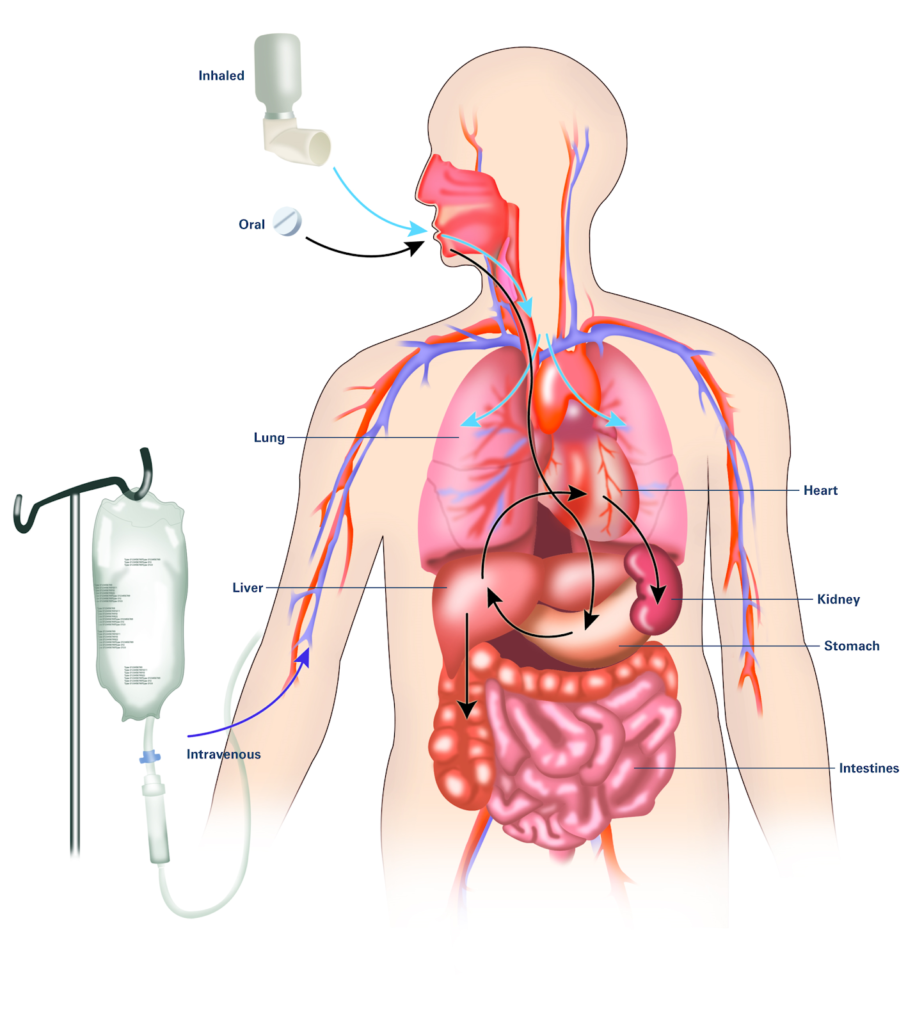
It is also important to consider the route of drug administration within the patient’s body. Many of us may have been prescribed oral antibiotics and have simply filled our prescription and completed the drug regimen within the comfort of our own homes. However, there are many types of infections or disease processes that do not respond well to the use of oral antimicrobial therapy. For these diseases, patients may require intravenous or intramuscular injections. Patients requiring intravenous or intramuscular injections may need to be hospitalized, have home health nursing arranged, or travel to the hospital/clinic for their therapy. Concerns with treatment compliance exists with all routes of administration. For more information about considerations regarding routes of administration, refer to Chapter 1 on absorption. See Figure 3.7[4] for an illustration of three common routes of medication within the body.
Drug Interactions
For the optimum treatment of select infections, two antibacterial drugs may be administered together. Concurrent drug administration produces a synergistic interaction that is better than the efficacy of either drug alone. In this case, TWO is truly better than ONE! A classic example of synergistic drug combinations is trimethoprim and sulfamethoxazole (Bactrim). Individually, these two drugs provide only bacteriostatic inhibition of bacterial growth, but combined, the drugs are bactericidal. [5]
Although synergistic drug interactions provide a benefit to the patient, antagonistic interactions produce harmful effects. Antagonism can occur between two antimicrobials or between antimicrobials and non-antimicrobials being used to treat other conditions. The effects vary depending on the drugs involved, but antagonistic interactions cause diminished drug activity, decreased therapeutic levels due to elevated metabolism and elimination, or increased potential for toxicity due to decreased metabolism and elimination.
Let’s consider an example of these antagonistic interactions.
Many antibacterials are absorbed most effectively from the acidic environment within the stomach. However, if a patient takes antacids, the antacids increase the pH of the stomach and negatively impact the absorption of the antibacterial, thus decreasing their effectiveness in treating an infection.
Interactive Activity
- "Concentration_vs_number_of_half-life_periodes.png" by OPPSD is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Microbiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction. ↵
- This work is a derivative of Microbiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction. ↵
- "A drug's life in the body (with labels)" by National Institute of General Medical Sciences Image and Video Gallery is licensed under CC NC-SA 3.0 ↵
- This work is a derivative of Microbiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction. ↵
Non-opioid analgesics include acetaminophen and nonsteroidal antiinflammatory drugs (NSAIDS).
Acetaminophen
Mechanism of Action
Acetaminophen inhibits the synthesis of prostaglandins that may serve as mediators of pain and fever primarily in the CNS.[1]
Indications for Use
Acetaminophen is used to treat mild pain and fever; however, it does not have anti-inflammatory properties.
Nursing Considerations Across the Lifespan
Acetaminophen is safe for all ages and can be administered using various routes.
Geriatric populations should not exceed 3000 mg in 24 hours, and chronic alcoholics should not exceed 2000 mg in 24 hours due to the risk for hepatoxicity.
Adverse/Side Effects
Adverse effects include skin reddening, blisters, rash, and hepatotoxicity.
Severe liver damage may occur if a patient:
- takes more than 4,000 mg of acetaminophen in 24 hours (3200 mg for geriatric adults, 2000 mg for chronic alcoholics)
- takes with other drugs containing acetaminophen
- consumes 3 or more alcoholic drinks every day while using this product.[2]
Some medications are combined with acetaminophen and are prescribed “as needed,” so the nurse must calculate the cumulative dose of acetaminophen over the previous 24-hour period. For example, Percocet 5/325 contains a combination of oxycodone 5 mg and acetaminophen 325 mg and could be ordered 1-2 tablets every 4-6 hours as needed for pain. If 2 tablets are truly administered every 4 hours over a 24-hour period, this would add up to 3900 mg of acetaminophen, which would exceed the recommended guidelines for a geriatric patient and could cause liver damage.
If overdose occurs, the antidote is acetylcysteine.
Patient Teaching & Education
Medications should be taken as directed and the dosing schedule should be adhered to appropriately. Patients should not take the medication for greater than 10 days. Additionally, patients should avoid taking alcohol while using these medications. If a rash occurs, this should be reported to the healthcare provider and the medication should be promptly stopped. Use of medications may interfere with blood glucose monitoring. If a fever lasts longer than three days or exceeds 39.5 C, this should be reported to the healthcare provider.[3]
Now let’s take a closer look at the medication grid on acetaminophen in Table 10.6a.[4],[5]',footnote]Centers for Disease Control and Prevention. (2019, August 28). Opioid overdose, CDC guideline for prescribing opioids for chronic pain. https://www.cdc.gov/drugoverdose/prescribing/guideline.html[/footnote] Medication grids are intended to assist students to learn key points about each medication. Because information about medication is constantly changing, nurses should always consult evidence-based resources to review current recommendations before administering specific medication. Basic information related to each class of medication is outlined below. Detailed information on a specific medication can be found for free at Daily Med at https://dailymed.nlm.nih.gov/dailymed/index.cfm. On the home page, enter the drug name in the search bar to read more about the medication. Prototype/generic medications listed in the grids below are also hyperlinked directly to a Daily Med page.
Table 10.6a Acetaminophen Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Nonopioid analgesic
Antipyretic |
acetaminophen | Can be given orally, rectally, and IV
Assess pain prior to and after administration Administer with a full glass of water Maximum dose over 24-hour period: -4000 mg for adults, -3200 mg for geriatric patients -2000 mg for patients with chronic alcoholism |
Relief of mild pain and fever | Skin reddening
Blisters Rash Hepatic failure (liver damage) |
Critical Thinking Activity 10.6a
Your patient is admitted to the hospital with acute liver failure due to acetaminophen toxicity. Your patient reveals that they have had a cold for several days and have been taking over-the-counter cold medications and acetaminophen for a headache. They also mention that every night after work they drink a “few” beers.
What patient education about acetaminophen should be provided?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
Nonsteroidal Antiinflammatories (NSAIDs)
Nonsteroidal antiinflammatories have an analgesic effect, as well as antipyretic and antiinflammatory actions. Some, such as aspirin, also have an antiplatelet effect. Aspirin and other NSAIDs relieve pain by inhibiting the biosynthesis of prostaglandin by different forms of the COX enzyme. COX2 inhibitors are selective and only inhibit the COX-2 enzyme. As a result of the inhibition of COX1 by an NSAID, there is decreased protection of the stomach lining and gastric irritation and bleeding may occur. This section will discuss the following NSAIDs: aspirin, ibuprofen, ketorolac, and celecoxib.[6]
Aspirin
Mechanism of Action
Aspirin produces analgesia and reduces inflammation and fever by inhibiting the production of prostaglandins. It also decreases platelet aggregation.
Indications for Use
Aspirin is used for the treatment of mild pain and fever. Once daily dosages are also used to reduce the risk of heart attack and stroke.
Nursing Considerations Across the Lifespan
Aspirin is safe for adults and children older than 12 years of age.
Adverse/Side Effects
Adverse effects include GI upset, GI bleed, and tinnitus (ringing of the ears).
Allergy alert: Aspirin may cause a severe allergic reaction, which may include:
- hives
- facial swelling
- shock
- asthma (wheezing)
Stomach bleeding warning: This product contains an NSAID, which may cause severe stomach bleeding. The chance for bleeding is higher if a patient:
- takes a higher dose or takes it for a longer time than directed
- takes other drugs containing prescription or nonprescription NSAIDs (aspirin, ibuprofen, naproxen, or others)
- has had stomach ulcers or bleeding problems
- takes a blood thinning (anticoagulant) or steroid drug
- is age 60 or older
- has 3 or more alcoholic drinks every day while using this product
Aspirin is contraindicated if the patient has a bleeding disorder such as hemophilia or a recent history of bleeding in the stomach or intestine.
Patient Teaching & Education
Patients should avoid concurrent use of alcohol while taking medication to avoid gastric irritation. Additionally, they should report tinnitus, unusual bleeding, or fever lasting greater than 3 days to the healthcare provider.
Black Box Warning
Children or teenagers should not take aspirin to treat chickenpox or flu-like symptoms because of the risk of Reye’s Syndrome. Reye's Syndrome primarily occurs in children in conjunction with a viral illness; it can cause symptoms such as persistent vomiting, confusion or loss of consciousness and requires immediate medical attention.
Now let’s take a closer look at the medication grid on aspirin in Table 10.6b.[7],[8],[9],[10]
Table 10.6b Aspirin Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Nonopioid analgesic
(NSAID) Antipyretic |
aspirin |
Give orally Assess pain prior to and after administration Children under 12 years: do not use unless directed by a provider Take with a full glass of water and sit upright for 15-30 minutes after administration Take with food if the patient reports that aspirin upsets their stomach Do not crush, chew, break, or open an enteric-coated or delayed-release pill; it should be swallowed whole The chewable tablet form must be chewed before swallowing Should be stopped 7 days prior to surgery due to the risk of postoperative bleeding |
Treatment of mild pain and fever
Reduces the risk of heart attack and stroke |
GI upset
GI bleeding Tinnitus |
Critical Thinking Activity 10.6b
A patient asks why aspirin is given to prevent a heart attack or stroke.
What is the nurse’s response?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
Ibuprofen
Mechanism of Action
Ibuprofen inhibits prostaglandin synthesis.
Indications for Use
Ibuprofen is used to treat mild to moderate pain and fever, inflammatory disorders including rheumatoid arthritis and osteoarthritis, and pain associated with dysmenorrhea.
Nursing Considerations Across the Lifespan
Ibuprofen is safe for infants 6 months or older. It is especially important not to use ibuprofen during the last 3 months of pregnancy unless directed to do so by a doctor because it may cause complications during delivery or in the unborn child.
Adverse/Side Effects
Adverse effects include headache, GI bleed, constipation, dyspepsia, nausea, vomiting, Steven-Johnson syndrome, and renal failure.
Allergy alert: Ibuprofen may cause a severe allergic reaction, especially in people allergic to aspirin. Symptoms may include:
- hives
- facial swelling
- asthma (wheezing)
- shock
- skin reddening
- rash
- blisters
Patient Teaching & Education
Patients should consume the medication with a full glass of water and remain upright for 30 minutes following medication administration. They should avoid the use of alcohol while taking this medication. Patients should be advised to not take the medication for longer than 10 days. If the patient notices rash, visual changes, tinnitus, weight gain, or influenza-like symptoms, these should be reported to the healthcare provider immediately.[11]
Stomach bleeding warning:
This product contains a nonsteroidal anti-inflammatory drug (NSAID), which may cause severe stomach bleeding. The chance for bleeding is higher if the patient:
- is age 60 or older
- has had stomach ulcers or bleeding problems
- takes a blood thinning (anticoagulant) or steroid drug
- takes other drugs containing prescription or nonprescription NSAIDs (aspirin, ibuprofen, naproxen, or others)
- has 3 or more alcoholic drinks every day while using this product
- takes more or for a longer time than directed
Heart attack and stroke warning:
All NSAIDs, except aspirin, increase the risk of heart attack, heart failure, and stroke. These can be fatal. The risk is higher if the patient takes more than is directed or takes it for longer than directed.
Black Box Warning
Ibuprofen is contraindicated for the treatment of perioperative pain after coronary artery bypass graft.
Now let’s take a closer look at the medication grid on ibuprofen in Table 10.6c.[12],[13]
Table 10.6c Ibuprofen Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Nonopioid analgesic
NSAID Antipyretic |
ibuprofen | Given parenterally and orally
Assess pain prior to and after administration May take with food or milk if stomach upset occurs Stay well hydrated to prevent renal failure Assess patient for signs of GI bleed Assess for skin rash Monitor BUN, serum creatinine, CBC, and liver function test Do not administer to patients who are allergic to aspirin or other NSAIDs |
To relieve mild pain and to reduce fever | Headache
GI bleed Constipation Dyspepsia Nausea Vomiting Steven-Johnson syndrome Renal failure |
Critical Thinking Activity 10.6c
A patient who is a chronic alcoholic asks if it is okay to take ibuprofen for knee pain.
What is the nurse’s best response?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
Ketorolac
Ketorolac is an NSAID that is commonly used to treat “breakthrough” pain that occurs during the treatment of severe acute pain being treated with opioids.
Mechanism of Action
Ketorolac inhibits prostaglandin synthesis.
Indications for Use
Ketorolac is indicated for the short-term (up to 5 days in adults) management of moderate to severe acute pain that requires analgesia at the opioid level.
Nursing Considerations Across the Lifespan
Ketorolac is safe for adults. This dose should be reduced for patients ages 65 and over.
Adverse/Side Effects
Adverse effects include drowsiness, headache, GI bleed, abnormal taste, dyspepsia, nausea, Steven-Johnson syndrome, edema, and renal failure.
Patient Teaching & Education
The use of ketorolac may cause dizziness of drowsiness. Patients should also avoid alcohol or other aspirin-containing products unless directed by their healthcare provider. If the patient notices rash, visual changes, tinnitus, weight gain, or influenza-like symptoms, these should be reported to the healthcare provider immediately.[14]
Gastrointestinal Risk
Ketorolac tromethamine (IV form) can cause peptic ulcers, gastrointestinal bleeding, and/or perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Therefore, ketorolac tromethamine is contraindicated in patients with active peptic ulcer disease, in patients with recent gastrointestinal bleeding or perforation, and in patients with a history of peptic ulcer disease or gastrointestinal bleeding. Elderly patients are at greater risk for serious gastrointestinal events.
Cardiovascular Thrombotic Events
Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use.
Ketorolac tromethamine is contraindicated for patients who have recently received coronary artery bypass graft (CABG) surgery.
Renal Risk
Ketorolac tromethamine is contraindicated in patients with advanced renal impairment and in patients at risk for renal failure due to volume depletion.
Risk of Bleeding
Ketorolac tromethamine inhibits platelet function and is, therefore, contraindicated in patients with suspected or confirmed cerebrovascular bleeding, hemorrhagic diathesis, incomplete hemostasis, and a high risk of bleeding. Ketorolac tromethamine is contraindicated as a prophylactic analgesic before any major surgery.
Hypersensitivity Reactions
Hypersensitivity reactions ranging from bronchospasm to anaphylactic shock have occurred and appropriate counteractive measures must be available when administering the first dose of ketorolac. Ketorolac tromethamine is contraindicated in patients with previously demonstrated hypersensitivity to ketorolac tromethamine or who have had allergic manifestations to aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs).
Now let’s take a closer look at the medication grid on ketorolac in Table 10.6d.[15],[16]
Table 10.6d Ketorolac Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Nonopioid analgesic
NSAID |
ketorolac | Given orally, parenterally and as an ophthalmic solution
Assess pain prior to and after administration Therapy should always be given initially by the IM or IV route; then use the oral route as a continuation of parenteral therapy Stay well hydrated to prevent renal failure Assess patient for signs of GI bleed Assess for skin rash Monitor BUN, serum creatinine, CBC, and liver function tests Do not administer before any major surgery Do not administer to patients who are allergic to aspirin or other NSAIDs |
To relieve moderate pain short term (not to exceed 5 days) | Drowsiness
Headache GI bleed Abnormal taste Dyspepsia Nausea Steven-Johnson syndrome Edema Renal failure |
Critical Thinking Activity 10.6d
Ketorolac IV was administered to a patient for severe pain (rated as “8”) due to a back injury.
When should the effectiveness of the medication be evaluated?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
Celecoxib
Celecoxib is a COX-2 inhibitor.
Mechanism of Action
Celecoxib specifically inhibits the enzyme COX-2 that is required for the synthesis of prostaglandins.
Indications for Use
Celecoxib is used to treat the pain associated with osteoarthritis, rheumatoid arthritis (including juvenile), and ankylosing spondylitis. It also relieves the pain associated with dysmenorrhea.
Nursing Considerations Across the Lifespan
Celecoxib is safe for children 2 years or older. Dosage adjustment is required for patients with hepatic impairment (see Black Box Warning).
Adverse/Side Effects
Adverse effects include hypertension, peripheral edema, increased liver enzymes, abdominal pain, dyspepsia, gastroesophageal reflux disease, vomiting, and diarrhea.
There are Black Box Warnings for increased risk of cardiovascular (CV) events and gastrointestinal bleeding, ulceration, and perforation. See more information about each condition below.
Patient Teaching & Education
Patients should take medication as directed and use the lowest effective dose for the shortest period of time. If signs of GI toxicity occur, these should be reported immediately to the healthcare provider.[17]
Cardiovascular Thrombotic Events
Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in the treatment and may increase with duration of use. Celecoxib capsules are contraindicated in patients who have recently received coronary artery bypass graft (CABG) surgery.
Gastrointestinal Bleeding, Ulceration, and Perforation
NSAIDs cause an increased risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at greater risk for serious (GI) events.
Now let’s take a closer look at the medication grid on celecoxib in Table 10.6e.[18],[19]
Table 10.6e Celecoxib Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| NSAIDs
COX-2 inhibitor |
celecoxib | May be given with or without food
May sprinkle capsules on applesauce and ingest immediately with water Monitor patients for signs and symptoms of Steven-Johnson syndrome Monitor for signs and symptoms of GI bleed, hypertension, and heart failure Monitor liver enzymes |
To decrease pain and inflammation caused by arthritis or spondylitis | Hypertension
Peripheral edema Increased liver enzymes Abdominal pain, dyspepsia, gastroesophageal reflux disease, vomiting, and diarrhea Cardiovascular thrombotic events GI bleeding, ulceration and perforation Hepatotoxicity Hypertension Heart failure and edema Renal toxicity and hyperkalemia Anaphylactic reactions Serious skin reactions Hematologic toxicity |
Critical Thinking Activity 10.6e
A patient has been prescribed celecoxib for their arthritic pain.
What patient teaching does the nurse plan to provide?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
Medications used as adjuvant analgesics have been developed for other purposes but were later found to be effective to treat pain. Examples of adjuvant medications include gapapentin (an anticonvulsant) and amitriptyline (a tricyclic antidepressant). Additional information about these specific medications can be found in the "Central Nervous System" chapter. Muscle relaxants are also considered an adjuvant analgesic and are used for various musculoskeletal disorders such as multiple sclerosis. Three different types of muscle relaxants will be discussed below: baclofen, cyclobenzaprine, and tizanidine.
Baclofen
Mechanism of Action
Baclofen inhibits reflexes at the spinal level.
Indications for Use
Baclofen is used to treat muscle symptoms, such as spasm, pain, and stiffness, caused by multiple sclerosis, spinal cord injuries, or other spinal cord disorders.
Nursing Considerations Across the Lifespan
Baclofen is safe for patients 12 years and older.
Adverse/Side Effects
Adverse effects include drowsiness, dizziness or lightheadedness, confusion, nausea, constipation, and muscle weakness.
Abrupt Drug Withdrawal: Hallucinations and seizures have occurred on abrupt withdrawal of baclofen. Therefore, except for serious adverse reactions, the dose should be reduced slowly when the drug is discontinued.
Impaired Renal Function: Because baclofen is primarily excreted unchanged through the kidneys, it should be given with caution, and it may be necessary to reduce the dosage.
Signs and symptoms of overdose include vomiting, muscular hypotonia, drowsiness, accommodation disorders of the eye, coma, respiratory depression, and seizures.
Patient Teaching & Education
The medication should be taken as directed and abrupt withdrawal of the medication should be avoided. It may cause dizziness or drowsiness. Patients should be advised to change positions slowly because of the potential orthostatic changes that may occur. Additionally, patients should avoid concurrent use with alcohol or other CNS depressants.[20]
Now let’s take a closer look at the medication grid on baclofen in Table 10.8a.[21],[22]
Table 10.8a Baclofen Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration
Considerations |
Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Skeletal muscle relaxant and antispasticity agent | baclofen | Given parantally and orally
Administer orally with milk or food to minimize gastric upset Assess for muscle spasticity before and during therapy Observe patient for drowsiness For intrathecal administration monitor patient closely during test dose and titration and have resuscitative equipment available |
To relieve muscle spasms and spasticity | Drowsiness
Confusion Dizziness or light-headedness Nausea Constipation Muscle weakness |
Critical Thinking Activity 10.8a
A patient just started taking baclofen for muscle spasticity due to multiple sclerosis.
What teaching should the nurse provide?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
Cyclobenzaprine
Mechanism of Action
Cyclobenzaprine reduces tonic somatic muscle activity at the level of the brainstem. It is structurally similar to tricyclic antidepressants.
Indications for Use
Cyclobenzaprine is used to treat acute muscle spasms.
Nursing Considerations Across the Lifespan
Cyclobenzaprine is safe for patients 15 years and older. Use cautiously with geriatric patients, patients with hepatic impairment, and those who take antidepressants and other CNS depressants.
In the elderly, the frequency and severity of adverse events associated with the use of cyclobenzaprine, with or without concomitant medications, are increased. In elderly patients, cyclobenzaprine should be initiated with a 5 mg dose and titrated slowly upward.
Adverse/Side Effects
Adverse effects include dizziness, drowsiness, dry mouth, urinary retention, serotonin syndrome with antidepressant use, or increased sedation with other CNS depressants.
Patient Teaching & Education
The medication should be taken as directed. It may cause dizziness or drowsiness. Patients should be advised to change positions slowly because of the potential orthostatic changes that may occur. Additionally, patients should avoid concurrent use with alcohol or other CNS depressants. Patients should be aware that constipation may occur as a side effect of medication therapy and increased fluid intake may assist in preventing complications.[23]
Serotonin Syndrome
The development of a potentially life-threatening serotonin syndrome has been reported with cyclobenzaprine hydrochloride when used in combination with other drugs, such as selective serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), tramadol, bupropion, meperidine, verapamil, or MAO inhibitors (MAOIs). The concomitant use of cyclobenzaprine hydrochloride with MAO inhibitors is contraindicated.
Serotonin syndrome symptoms may include mental status changes (e.g., confusion, agitation, hallucinations), autonomic instability (e.g., diaphoresis, tachycardia, labile blood pressure, hyperthermia), neuromuscular abnormalities (e.g., tremor, ataxia, hyperreflexia, clonus, muscle rigidity), and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Treatment with cyclobenzaprine hydrochloride and any concomitant serotonergic agents should be discontinued immediately if the above reactions occur, and supportive symptomatic treatment should be initiated. If concomitant treatment with cyclobenzaprine hydrochloride and other serotonergic drugs is clinically warranted, careful observation is advised, particularly during treatment initiation or dose increases.
General
Because of its atropine-like action, cyclobenzaprine hydrochloride should be used with caution in patients with a history of urinary retention, angle-closure glaucoma, increased intraocular pressure, and in those taking anticholinergic medication.
Impaired Hepatic Function
The plasma concentration of cyclobenzaprine is increased in patients with hepatic impairment.
Cyclobenzaprine, especially when used with alcohol or other CNS depressants, may impair mental and/or physical abilities required for performance of hazardous tasks, such as operating machinery or driving a motor vehicle.
Now let’s take a closer look at the medication grid on cyclobenzaprine in Table 10.8b.[24],[25]
Table 10.8b Cyclobenzaprine Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Skeletal muscle relaxant | cyclobenzaprine | May be administered with meals to minimize GI upset
Assess patient for pain and muscle stiffness Use cautiously with antidepressants and other CNS depressants |
Reduction of muscle spasms | Dizziness
Drowsiness Dry mouth Urinary retention Serotonin syndrome |
Critical Thinking Activity 10.8b
A patient asks if they can drive their car while taking cyclobenzaprine.
What is the nurse’s best response?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
Tizanidine
Mechanism of Action
Tizanidine acts as an agonist at central alpha-adrenergic receptor sites. It reduces spasticity by increasing presynaptic inhibition of motor neurons.
Indications for Use
Tizanidine is used to treat increased muscle tone, spasms, and spasticity.
Nursing Considerations Across the Lifespan
Tizanidine is safe for adults. Dosage adjustment may be required for the geriatric population.
Adverse/Side Effects
Adverse effects include somnolence, dry mouth, hypotension, bradycardia, dizziness, fatigue, weakness or asthenia, hallucinations, liver function test abnormality, and hepatotoxicity.
Patient Teaching & Education
The medication should be taken as directed. It may cause dizziness or drowsiness. Patients should be advised to change positions slowly because of the potential orthostatic changes that may occur. Additionally, patients should avoid concurrent use with alcohol or other CNS depressants.[26]
Now let’s take a closer look at the medication grid on tizanidine in Table 10.8c.[27],[28],[29]
Table 10.8c Tizanidine Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Antispasticity | tizanidine | Given orally
May be given with or without food Assess muscle spasticity before and during therapy Assess blood pressure and pulse Monitor for sedation Assess liver function |
Reduction of muscle spasms and spasticity | Somnolence
Dry mouth Hypotension Bradycardia Dizziness Fatigue Weakness or asthenia Hallucinations Liver function test abnormality and hepatotoxicity |
Critical Thinking Activity 10.8c
A patient asks, “Why should I not drink alcohol with tizanidine?”
What is the nurse’s best response?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
Medications used as adjuvant analgesics have been developed for other purposes but were later found to be effective to treat pain. Examples of adjuvant medications include gapapentin (an anticonvulsant) and amitriptyline (a tricyclic antidepressant). Additional information about these specific medications can be found in the "Central Nervous System" chapter. Muscle relaxants are also considered an adjuvant analgesic and are used for various musculoskeletal disorders such as multiple sclerosis. Three different types of muscle relaxants will be discussed below: baclofen, cyclobenzaprine, and tizanidine.
Baclofen
Mechanism of Action
Baclofen inhibits reflexes at the spinal level.
Indications for Use
Baclofen is used to treat muscle symptoms, such as spasm, pain, and stiffness, caused by multiple sclerosis, spinal cord injuries, or other spinal cord disorders.
Nursing Considerations Across the Lifespan
Baclofen is safe for patients 12 years and older.
Adverse/Side Effects
Adverse effects include drowsiness, dizziness or lightheadedness, confusion, nausea, constipation, and muscle weakness.
Abrupt Drug Withdrawal: Hallucinations and seizures have occurred on abrupt withdrawal of baclofen. Therefore, except for serious adverse reactions, the dose should be reduced slowly when the drug is discontinued.
Impaired Renal Function: Because baclofen is primarily excreted unchanged through the kidneys, it should be given with caution, and it may be necessary to reduce the dosage.
Signs and symptoms of overdose include vomiting, muscular hypotonia, drowsiness, accommodation disorders of the eye, coma, respiratory depression, and seizures.
Patient Teaching & Education
The medication should be taken as directed and abrupt withdrawal of the medication should be avoided. It may cause dizziness or drowsiness. Patients should be advised to change positions slowly because of the potential orthostatic changes that may occur. Additionally, patients should avoid concurrent use with alcohol or other CNS depressants.[30]
Now let’s take a closer look at the medication grid on baclofen in Table 10.8a.[31],[32]
Table 10.8a Baclofen Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration
Considerations |
Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Skeletal muscle relaxant and antispasticity agent | baclofen | Given parantally and orally
Administer orally with milk or food to minimize gastric upset Assess for muscle spasticity before and during therapy Observe patient for drowsiness For intrathecal administration monitor patient closely during test dose and titration and have resuscitative equipment available |
To relieve muscle spasms and spasticity | Drowsiness
Confusion Dizziness or light-headedness Nausea Constipation Muscle weakness |
Critical Thinking Activity 10.8a
A patient just started taking baclofen for muscle spasticity due to multiple sclerosis.
What teaching should the nurse provide?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
Cyclobenzaprine
Mechanism of Action
Cyclobenzaprine reduces tonic somatic muscle activity at the level of the brainstem. It is structurally similar to tricyclic antidepressants.
Indications for Use
Cyclobenzaprine is used to treat acute muscle spasms.
Nursing Considerations Across the Lifespan
Cyclobenzaprine is safe for patients 15 years and older. Use cautiously with geriatric patients, patients with hepatic impairment, and those who take antidepressants and other CNS depressants.
In the elderly, the frequency and severity of adverse events associated with the use of cyclobenzaprine, with or without concomitant medications, are increased. In elderly patients, cyclobenzaprine should be initiated with a 5 mg dose and titrated slowly upward.
Adverse/Side Effects
Adverse effects include dizziness, drowsiness, dry mouth, urinary retention, serotonin syndrome with antidepressant use, or increased sedation with other CNS depressants.
Patient Teaching & Education
The medication should be taken as directed. It may cause dizziness or drowsiness. Patients should be advised to change positions slowly because of the potential orthostatic changes that may occur. Additionally, patients should avoid concurrent use with alcohol or other CNS depressants. Patients should be aware that constipation may occur as a side effect of medication therapy and increased fluid intake may assist in preventing complications.[33]
Serotonin Syndrome
The development of a potentially life-threatening serotonin syndrome has been reported with cyclobenzaprine hydrochloride when used in combination with other drugs, such as selective serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), tramadol, bupropion, meperidine, verapamil, or MAO inhibitors (MAOIs). The concomitant use of cyclobenzaprine hydrochloride with MAO inhibitors is contraindicated.
Serotonin syndrome symptoms may include mental status changes (e.g., confusion, agitation, hallucinations), autonomic instability (e.g., diaphoresis, tachycardia, labile blood pressure, hyperthermia), neuromuscular abnormalities (e.g., tremor, ataxia, hyperreflexia, clonus, muscle rigidity), and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Treatment with cyclobenzaprine hydrochloride and any concomitant serotonergic agents should be discontinued immediately if the above reactions occur, and supportive symptomatic treatment should be initiated. If concomitant treatment with cyclobenzaprine hydrochloride and other serotonergic drugs is clinically warranted, careful observation is advised, particularly during treatment initiation or dose increases.
General
Because of its atropine-like action, cyclobenzaprine hydrochloride should be used with caution in patients with a history of urinary retention, angle-closure glaucoma, increased intraocular pressure, and in those taking anticholinergic medication.
Impaired Hepatic Function
The plasma concentration of cyclobenzaprine is increased in patients with hepatic impairment.
Cyclobenzaprine, especially when used with alcohol or other CNS depressants, may impair mental and/or physical abilities required for performance of hazardous tasks, such as operating machinery or driving a motor vehicle.
Now let’s take a closer look at the medication grid on cyclobenzaprine in Table 10.8b.[34],[35]
Table 10.8b Cyclobenzaprine Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Skeletal muscle relaxant | cyclobenzaprine | May be administered with meals to minimize GI upset
Assess patient for pain and muscle stiffness Use cautiously with antidepressants and other CNS depressants |
Reduction of muscle spasms | Dizziness
Drowsiness Dry mouth Urinary retention Serotonin syndrome |
Critical Thinking Activity 10.8b
A patient asks if they can drive their car while taking cyclobenzaprine.
What is the nurse’s best response?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
Tizanidine
Mechanism of Action
Tizanidine acts as an agonist at central alpha-adrenergic receptor sites. It reduces spasticity by increasing presynaptic inhibition of motor neurons.
Indications for Use
Tizanidine is used to treat increased muscle tone, spasms, and spasticity.
Nursing Considerations Across the Lifespan
Tizanidine is safe for adults. Dosage adjustment may be required for the geriatric population.
Adverse/Side Effects
Adverse effects include somnolence, dry mouth, hypotension, bradycardia, dizziness, fatigue, weakness or asthenia, hallucinations, liver function test abnormality, and hepatotoxicity.
Patient Teaching & Education
The medication should be taken as directed. It may cause dizziness or drowsiness. Patients should be advised to change positions slowly because of the potential orthostatic changes that may occur. Additionally, patients should avoid concurrent use with alcohol or other CNS depressants.[36]
Now let’s take a closer look at the medication grid on tizanidine in Table 10.8c.[37],[38],[39]
Table 10.8c Tizanidine Medication Grid
| Class/
Subclass |
Prototype-
generic |
Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Antispasticity | tizanidine | Given orally
May be given with or without food Assess muscle spasticity before and during therapy Assess blood pressure and pulse Monitor for sedation Assess liver function |
Reduction of muscle spasms and spasticity | Somnolence
Dry mouth Hypotension Bradycardia Dizziness Fatigue Weakness or asthenia Hallucinations Liver function test abnormality and hepatotoxicity |
Critical Thinking Activity 10.8c
A patient asks, “Why should I not drink alcohol with tizanidine?”
What is the nurse’s best response?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" sections at the end of the book.
As a nurse, you may care for a patient prior to surgery (preoperative), during surgery (perioperative), or after surgery (postoperative). One of your roles is to monitor your patient's vitals signs, paying close attention to respiratory status (respiratory rate, depth, quality, and SpO2). You will also assess LOC (level of consciousness) and pain level. Below is a description of the types of anesthetics.
Local
Local anesthetic is when a medication (e.g., lidocaine) is injected into the skin at the site of the procedure to achieve numbness for procedures like suturing.
Conscious Sedation
Conscious sedation is a combination of medications that allow the patient to be relaxed (midazolam) and free of pain (e.g., fentanyl) during a medical procedure (e.g., colonoscopy). This allows the patient to remain awake and aware, without feeling discomfort. The patient may or may not be able to speak or respond in this state.
General Anesthesia
General anesthesia is a medication-induced reversible unconsciousness with loss of protective reflexes. Arousal, even to painful stimuli, cannot occur. General anesthesia requires the establishment and maintenance of airway control.[40] Propofol is an example of an intravenous general anesthetic. The intravenous (IV) injection of propofol induces anesthesia within 40 seconds from the start of injection. [41]
Lightbulb Moment
Now let’s apply what you have learned!
Your 82-year-old postoperative patient is hard to arouse 30 minutes after you administered IV morphine. Their BP is 102/72, respirations are 8 and shallow and SpO2 is 88% on room air. Which of the following (with health care provider orders) are priority nursing actions? Select all that apply.
a) Administer oxygen
b) Administer naloxone
c) Insert a foley catheter
d) Increase IV fluid rate
e) Raise the head of the bed
Note: Answers to the Lightbulb Moment can be found in the "Answer Key" sections at the end of the book.
