6.3 Common Cardiac Disorders
Now that we have reviewed the basic anatomy and physiology concepts of the cardiovascular and renal system, let’s discuss some common cardiac disorders.
Hyperlipidemia
Cholesterol is a fat (also called a lipid) that your body needs to work properly. However, too much bad cholesterol can increase the risk for heart disease, stroke, and peripheral vascular disease. The medical term for high blood cholesterol is hyperlipidemia. There are many types of cholesterol (see Figure 6.16 for basic types of cholesterol.[1])
- Total cholesterol: All the cholesterols combined
- High density lipoprotein (HDL) cholesterol: Often called “good” cholesterol because it promotes the excretion of cholesterol. Exercise helps to increase HDL and remove cholesterol from the bloodstream
- Low density lipoprotein (LDL) cholesterol: Often called “bad” cholesterol because it stores cholesterol in the bloodstream, which contributes to atherosclerosis
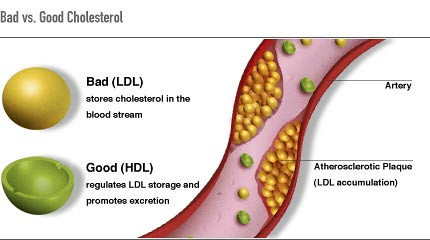
For many people, abnormal cholesterol levels are partly due to lifestyle choices, including a diet that is high in fat, being overweight, or lack of exercise. However, disorders can also be passed down through families that lead to abnormal cholesterol and triglyceride levels.[2] In addition to lifestyle modifications such as a low-fat diet and exercise, hyperlipidemia is treated with antilipidemic medication such as atorvastatin (Lipitor) to help prevent long-term complications.
Hypertension
Chronically elevated blood pressure is known clinically as hypertension. High blood pressure is treated with lifestyle changes and medication. New American Heart Association guidelines state that hypertension should be treated at 130/80 mm Hg rather than the previous standard of 140/90.[3] See Figure 6.17[4] for an image of a health care professional obtaining an accurate blood pressure reading that will be used to determine a treatment plan for the patient.

About 68 million Americans currently suffer from hypertension. Unfortunately, hypertension is often a silent disorder, meaning no symptoms occur until complications happen, so patients may fail to recognize the seriousness of their condition and fail to follow their treatment plan. The result is often a heart attack or stroke. Hypertension may also lead to an aneurysm (ballooning of a blood vessel caused by a weakening of the wall), peripheral arterial disease (obstruction of vessels in peripheral regions of the body), myocardial infarction, chronic kidney disease, or heart failure.[5]
Many cardiovascular medications are commonly used to treat hypertension such as diuretics, ACE inhibitors, beta blockers, and calcium channel blockers.
Thrombi and Emboli
Thrombi are most commonly caused by vessel damage to the endothelial lining, which activates the clotting mechanism. A thrombus can seriously impede blood flow to tissue or organs. Deep vein thrombosis (DVT) can occur when blood in the veins, particularly in the legs, remains stationary for long periods, such as during and after surgery. See Figure 6.18[6] for an image of a patient experiencing typical symptoms of a DVT, including unilateral edema and redness.[7]

When a portion of a thrombus breaks free from the vessel wall and enters the circulation, it is referred to as an embolus. An embolus that is carried through the bloodstream can be large enough to block a vessel critical to a major organ. When it becomes trapped, an embolus is called an embolism. In the heart, brain, or lungs, an embolism may cause a heart attack, a cerebrovascular accident (CVA) or otherwise known as a stroke, or a pulmonary embolism. These are medical emergencies.
Medications such as aspirin and warfarin are used to prevent the formation of clots in people who are at risk. Heparin is a medication that can be used to prevent or treat clots, and tPA is used to dissolve severe clots causing ischemia in the brain, heart, or lungs.[8]
Atherosclerosis
Arteriosclerosis begins with injury to the endothelium of an artery, which may be caused by irritation from high blood glucose, infection, tobacco use, excessive blood lipids, and other factors. Injured artery walls causes inflammation. As inflammation spreads into the artery wall, it weakens and scars it, leaving it stiff. Circulating triglycerides and cholesterol can seep between the damaged lining cells and become trapped within the artery wall, where they are joined by leukocytes, calcium, and cellular debris. Eventually, this buildup, called plaque, can narrow arteries enough to impair blood flow. The term for this condition, atherosclerosis, describes the plaque deposits. See Figure 6.19[9] for an illustration of atherosclerosis.[10]
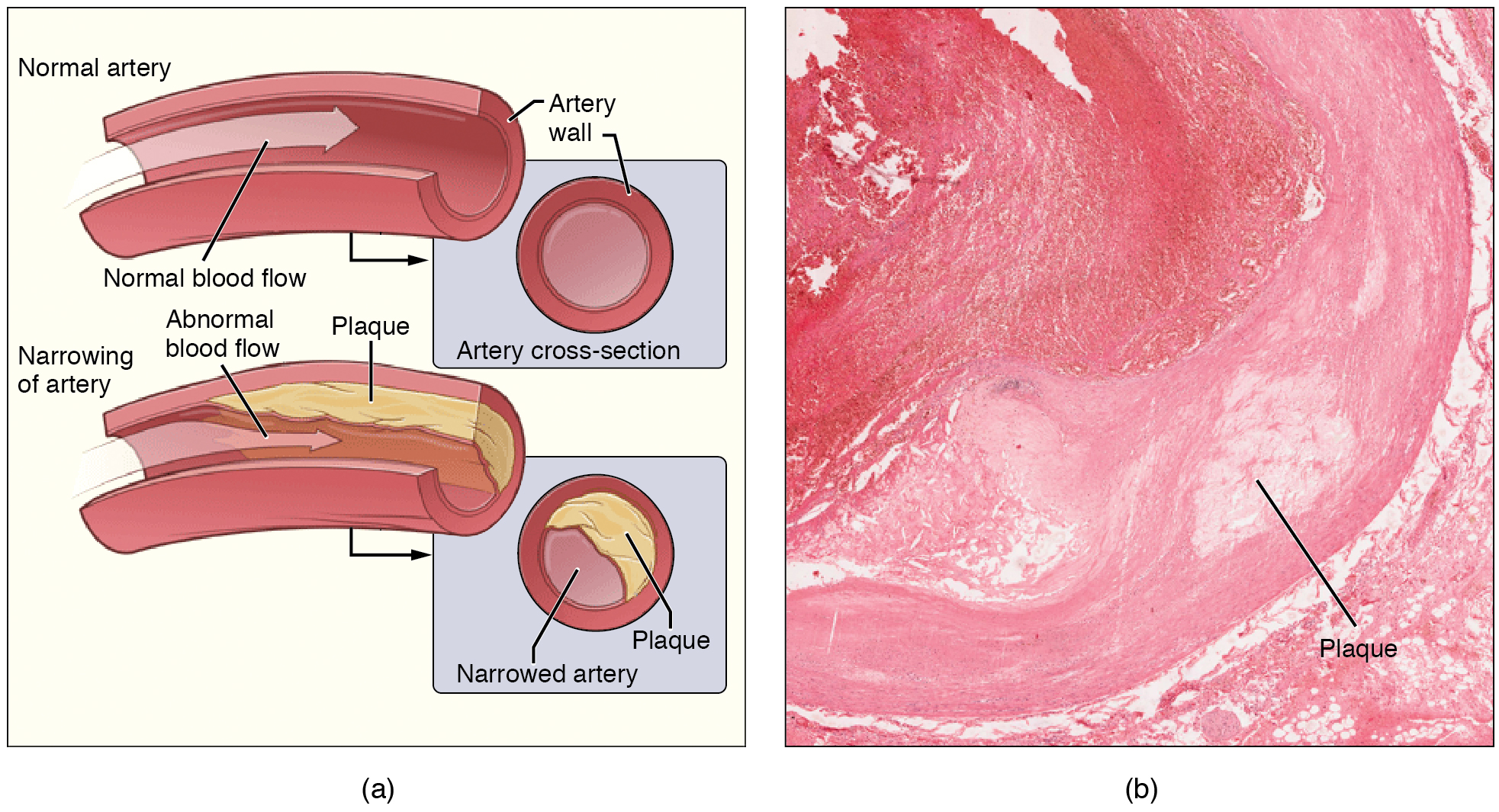
Sometimes a plaque can rupture, causing microscopic tears in the artery wall that allow blood to leak into the tissue on the other side. When this happens, platelets rush to the site to clot the blood. This clot can further obstruct the artery and—if it occurs in a coronary or cerebral artery—cause a sudden heart attack or stroke. Alternatively, plaque can also break off and travel through the bloodstream as an embolus until it blocks a more distant, smaller artery.
Even without total blockage, narrowed vessels lead to ischemia (reduced blood flow to the tissue region “downstream” of the narrowed vessel). Ischemia can lead to hypoxia (decreased supply of oxygen to the tissues), causing a myocardial infarction or cerebrovascular accident.
Treatment of atherosclerosis includes lifestyle changes, such as weight loss, smoking cessation, regular exercise, and adoption of a diet low in sodium and saturated fats. Antilipemic medications such as atorvastatin are prescribed to reduce cholesterol and help prevent atherosclerosis.
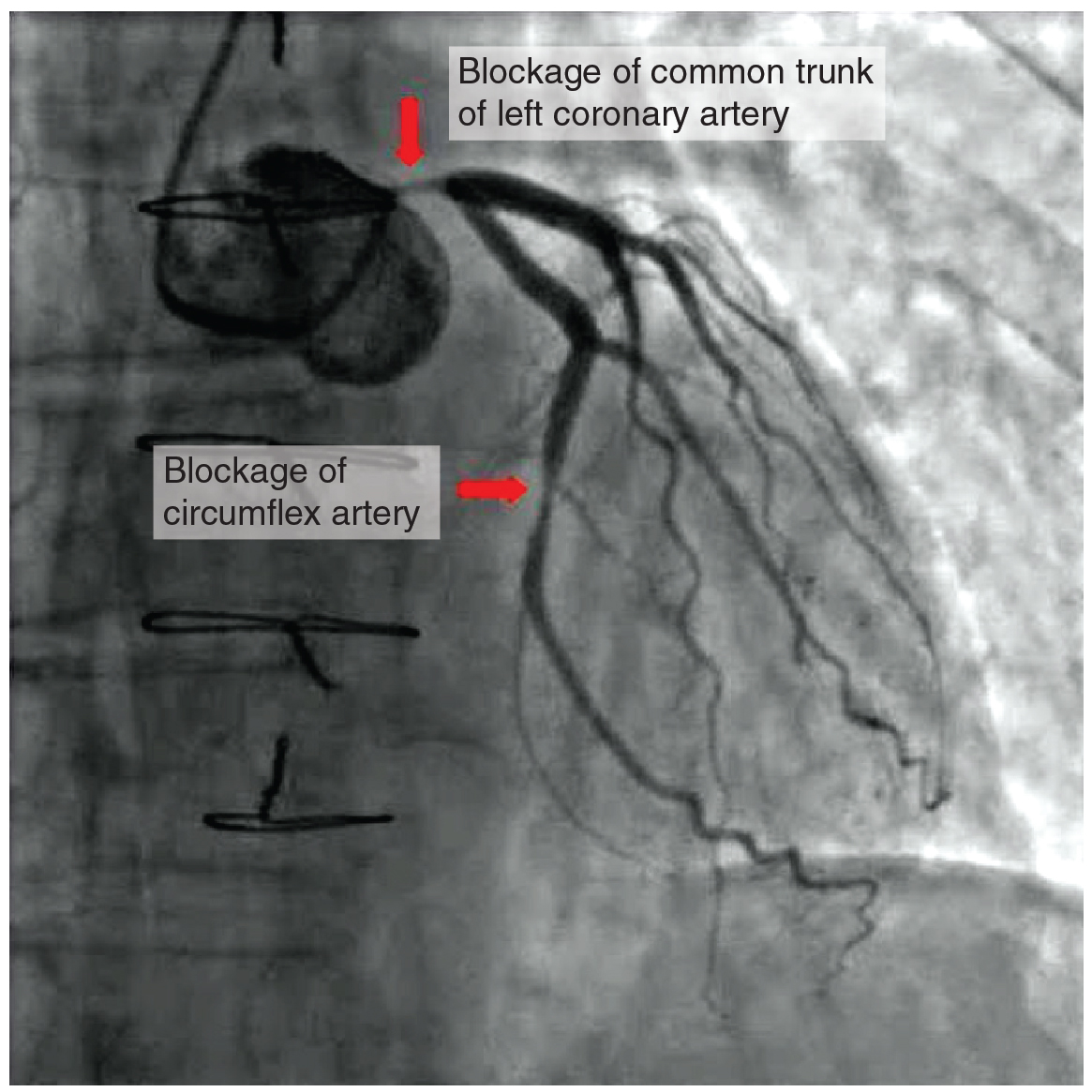
Coronary Artery Disease
Coronary artery disease is the leading cause of death worldwide. It occurs when atherosclerosis within the walls of the coronary arteries obstructs blood flow. As the coronary blood vessels become blocked with plaque, the flow of blood to the tissues is restricted, causing the cardiac cells to receive insufficient amounts of oxygen, which can cause pain called angina. Figure 6.20[11] shows the blockage of coronary arteries highlighted by the injection of dye. Some individuals with coronary artery disease report pain radiating from the chest called angina, but others, especially women, may remain asymptomatic or have alternative symptoms of neck, jaw, shoulder, upper back, or abdominal pain. If untreated, coronary artery disease can lead to a myocardial infarction (heart attack). Risk factors include smoking, family history, hypertension, obesity, diabetes, lack of exercise, stress, and hyperlipidemia. Treatments may include medication, changes to diet and exercise, a coronary angioplasty with a balloon catheter, insertion of a stent, or coronary bypass procedure.[12]
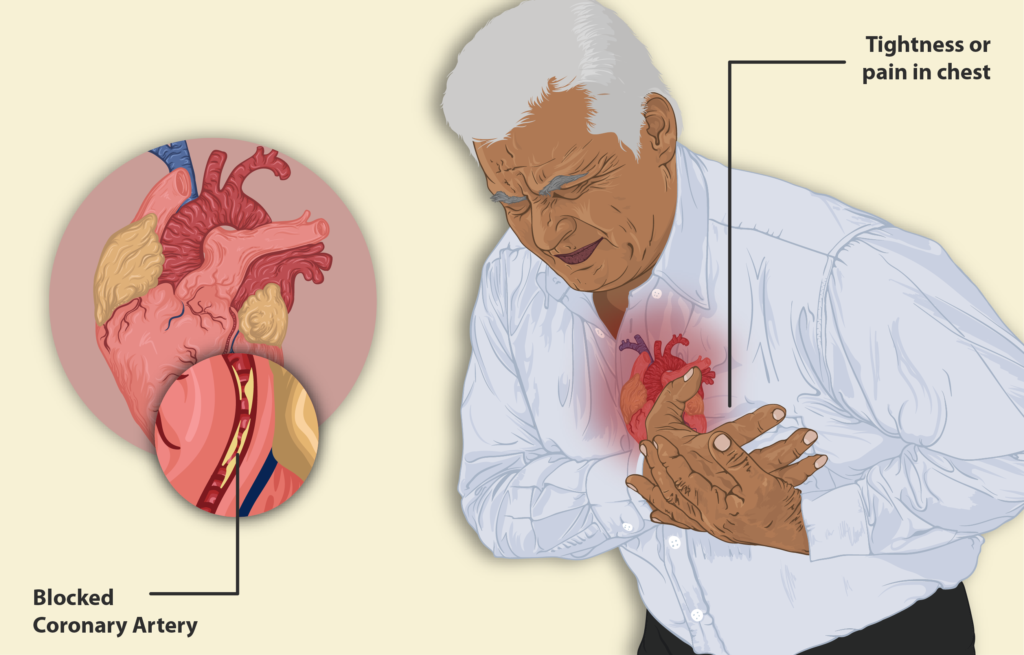
Myocardial Infarction
Myocardial infarction (MI) is the medical term for what is commonly referred to as a “heart attack.” It results from a lack of blood flow and oxygen to a region of the heart, resulting in death of the cardiac muscle cells. An MI often occurs when a coronary artery is blocked by the buildup of atherosclerotic plaque and becomes a thrombus or when a portion of an unstable atherosclerotic plaque travels through the coronary arterial system and lodges in one of the smaller vessels.
In the case of acute MI, there is often sudden pain beneath the sternum (retrosternal pain) called angina, often radiating down the left arm in male patients, but not as commonly in female patients (see Figure 6.21).[13] In addition, patients typically present with difficulty breathing and shortness of breath (dyspnea), irregular heartbeat (palpitations), nausea and vomiting, sweating (diaphoresis), anxiety, and fainting (syncope), although not all of these symptoms may be present. Many of the symptoms are shared with other medical conditions, including anxiety attacks and simple indigestion, so accurate diagnosis is critical for survival.
An MI can be confirmed by examining the patient’s ECG, which frequently reveals alterations in the ST and Q components. Immediate treatments for MI are required and include administering supplemental oxygen, aspirin, and nitroglycerin. Longer-term treatments may include injections of thrombolytic agents such as tPA that dissolve the clot, along with the anticoagulant heparin, a balloon angioplasty with stents to open blocked vessels, or bypass surgery to allow blood to pass around the site of blockage.[14]
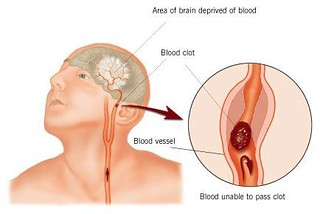
Cerebrovascular Accident (CVA)
The internal carotid arteries, along with the vertebral arteries, are the two primary suppliers of blood to the human brain. Given the central role and vital importance of the brain to life, it is critical that blood supply to this organ remains uninterrupted. However, blood flow may become obstructed due to atherosclerosis or an emboli that has traveled from elsewhere in the blood. For example, an arrhythmia called atrial fibrillation can cause clots to form in the heart that then move to the brain. When blood flow is interrupted, even for just a few seconds, a transient ischemic attack (TIA), or mini-stroke, may occur, resulting in loss of consciousness or temporary loss of neurological function. Loss of blood flow for longer periods produce irreversible brain damage or a stroke, also called a cerebrovascular accident (CVA).[15] There are two types of cerebrovascular accidents: ischemia and hemorrhagic. Ischemic strokes are caused by atherosclerosis or a blood clot that blocks the flow of blood to the brain (see Figure 6.22).[16] Eighty percent of strokes are ischemic. Hemorrhagic strokes are caused by a blood vessel that ruptures and bleeds into the brain. Risk factors for a stroke include smoking, high blood pressure, and cardiac arrhythmias. Treatment of a stroke depends on the cause.[17] Ischemic strokes are treated with thrombolytic medication such as tPA to dissolve the clot, whereas hemorrhagic strokes often require surgery to stop the bleeding.
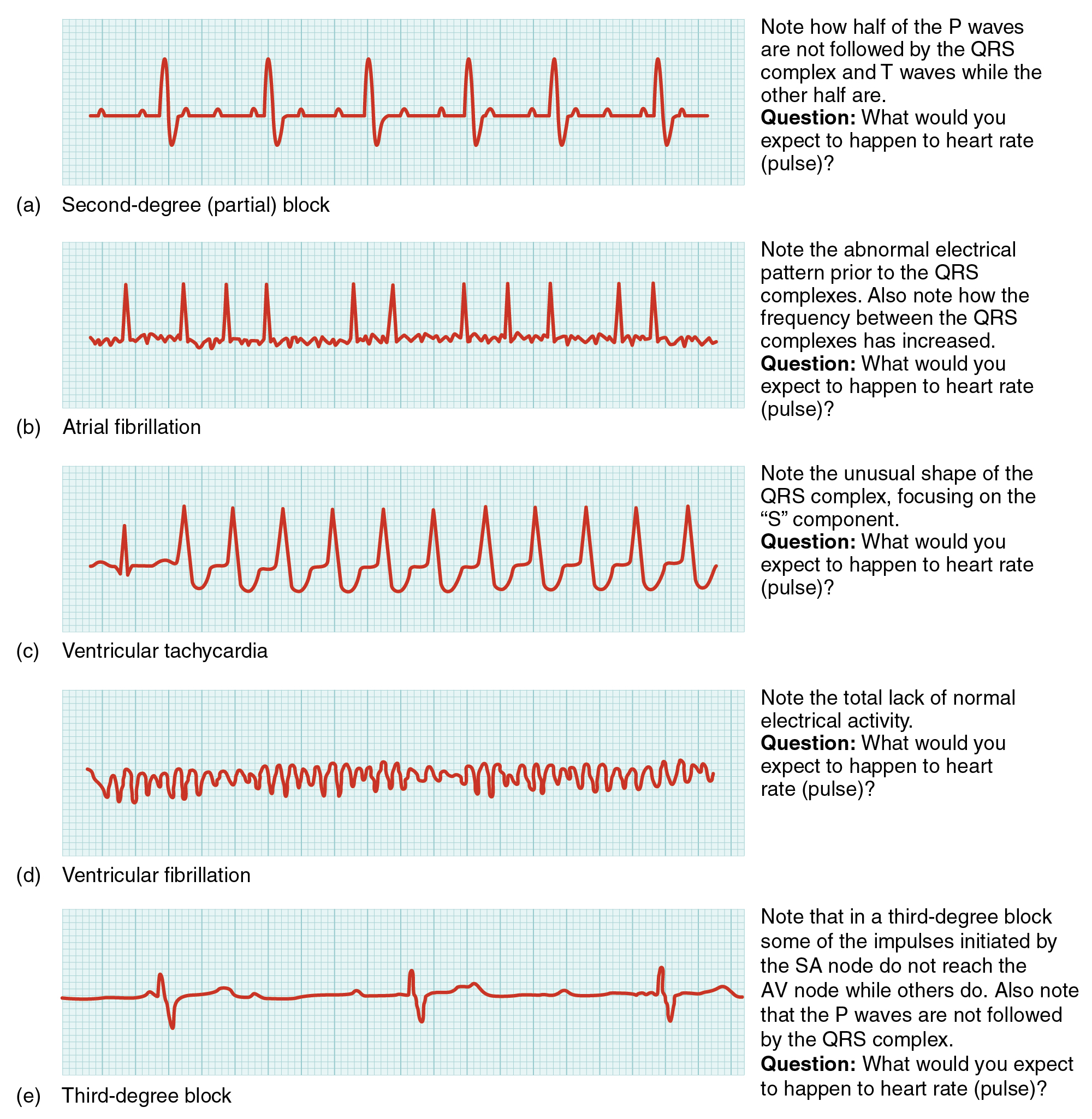
Arrhythmias
Occasionally, an area of the heart other than the SA node will initiate an impulse that will be followed by a premature contraction. Such an area is known as an ectopic focus. An ectopic focus may be stimulated by localized ischemia, exposure to certain drugs, elevated stimulation by both sympathetic or parasympathetic divisions of the autonomic nervous system, or several diseases or pathological conditions. Occasional occurrences are generally transitory and nonlife threatening, but if the condition becomes chronic, it may lead to either an arrhythmia, a deviation from the normal pattern of impulse conduction and contraction, or to fibrillation, an uncoordinated beating of the heart. Severe arrhythmias can lead to cardiac arrest, which is fatal if not treated within a few minutes. Abnormalities that may be detected by the ECGs are shown in Figure 6.23.[18] Antiarrhythmic medications such as sotalol, diltiazem, and amiodarone are used to treat arrhythmias.
Heart Failure
Heart failure is a condition in which the heart can’t pump enough blood to meet the body’s needs. Right-side heart failure occurs if the heart can’t pump enough blood to the lungs to pick up oxygen, whereas left-side heart failure occurs if the heart can’t pump enough oxygen-rich blood to the rest of the body. Heart failure is a very common condition with over 5.7 million people in the United States having this chronic condition. There is no cure, but the symptoms can be managed for several years with lifestyle modifications and several different types of medications. Causes of heart failure include hypertension, myocardial infarction, and other cardiac and respiratory diseases. Common symptoms of heart failure include peripheral edema and shortness of breath that occur as a result of fluid overload. Many patients are treated with diuretics to manage the symptoms of fluid overload and with antihypertensives to manage the blood pressure. Other medications such as digoxin and dobutamine may also be used to increase the contractility of the heart.[19]
- "máu nhiễm mỡ - cholesterol" by LÊ VĂN THẢO is licensed under CC BY-SA 2.0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c2019. High blood cholesterol levels; [reviewed 2018 February 22; updated 2018 March 28; cited 2019 November 29]. https://medlineplus.gov/ency/article/000403.htm. ↵
- Whelton, P.K., Carey R.M., Aronow W.S., et. al. (2018). 2017 Guideline for high blood pressure in adults. Journal of the American College of Cardiology, 71. https://www.acc.org/latest-in-cardiology/ten-points-to-remember/2017/11/09/11/41/2017-guideline-for-high-blood-pressure-in-adults. ↵
- "Monthly check up." by Bryan Mason is licensed under CC BY 2.0 ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of "Deep vein thrombosis of the right leg.jpg" by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- "2113ab Atherosclerosis.jpg" by OpenStax College is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/20-2-blood-flow-blood-pressure-and-resistance ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- "2016 Occluded Coronay Arteries.jpg" by OpenStax College is licensed under CC BY 3.0 ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- "A man having a Heart Attack.png" by https://www.myupchar.com/en is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- "Stroke Diagram" by ConstructionDealMkting is licensed under CC BY 2.0 ↵
- Anderson, P. & Townsend, T. (2015) Preventing high-alert medication errors in hospital patients. Nurse Today, 10(5). https://www.americannursetoday.com/wp-content/uploads/2015/05/ant5-CE-421.pdf ↵
- "Common ECG Abnormalities" by CNX OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/19-2-cardiac-muscle-and-electrical-activity ↵
- National Heart, Lung, and Blood, National Institute of Health (2019). Heart failure. https://www.nhlbi.nih.gov/health-topics/heart-failure ↵
